|


 |
| CASE REPORT |
|
| Year : 2012 | Volume
: 4
| Issue : 1 | Page : 27-31 |
|
|
Gas-less video-assisted thyroidectomy for a solitary thyroid nodule: technical report of the first case performed at a rural teaching hospital in India and review of literature
Sanoop K Zachariah
Department of Surgical Disciplines, MOSC Medical College, Kolenchery, Cochin, India
| Date of Web Publication | 5-Sep-2012 |
Correspondence Address:
Sanoop K Zachariah
Department of Surgical Disciplines, MOSC Medical College, Kolenchery, Cochin, Kerala - 682311
India
 Source of Support: None, Conflict of Interest: None
PMID: 23066460 
 Abstract Abstract | | |
Minimally invasive thyroidectomy is still in its phase of evolution with various techniques being practiced only in certain centers internationally. The conventional thyroidectomy performed by the Kocher's cervicotomy often leaves an undesirable scar over the neck, the size of which is usually around 8-10 cm long. The main aim of minimally invasive thyroid surgery is to minimize or avoid the scar over the neck. Endoscopic thyroid surgery in India, especially in the state of Kerala, is still in its infancy. Here, we describe the first case report of a modified technique of video-assisted thyroid surgery using a laparoscope and conventional open surgical instruments. Video-assisted thyroidectomy enables adequate visualization of the operative field and provides a magnified view of the vital structures like the parathyroid gland, the recurrent laryngeal nerve, and the thyroid vasculature. The procedure described here can be considered as a more cost-effective alternative to the conventional minimally invasive video-assisted thyroidectomy (MIVAT), and therefore is feasible in a rural setup. Keywords: Endoscopic thyroidectomy, minimally invasive thyroidectomy, thyroid surgery, video-assisted thyroidectomy
How to cite this article:
Zachariah SK. Gas-less video-assisted thyroidectomy for a solitary thyroid nodule: technical report of the first case performed at a rural teaching hospital in India and review of literature. J Surg Tech Case Report 2012;4:27-31 |
How to cite this URL:
Zachariah SK. Gas-less video-assisted thyroidectomy for a solitary thyroid nodule: technical report of the first case performed at a rural teaching hospital in India and review of literature. J Surg Tech Case Report [serial online] 2012 [cited 2016 Jun 10];4:27-31. Available from: http://www.jstcr.org/text.asp?2012/4/1/27/100350 |
 Introduction Introduction | |  |
The conventional thyroidectomy performed by the Kocher's cervicotomy often leaves an undesirable scar on the anterior neck, the size of which is usually around 8-10 cm long. Minimal access surgery for the head and neck is now gaining popularity. Various minimally invasive procedures for surgery of the thyroid gland have been recently proposed and practiced and published with the primary goal of minimizing or avoiding the scar over the neck. However, the most popular and widely adopted technique is the minimally invasive video-assisted thyroidectomy (MIVAT) pioneered in Italy by Miccoli and his team. [1] Here, we describe the first case report and also a modified technique of video-assisted thyroid surgery performed at a rural teaching hospital in South India where a large volume of open thyroid surgeries are done routinely.
 Case Report Case Report | |  |
A 24-year-old woman presented with a 1.5-cm solitary nodule of the right thyroid lobe. Fine needle aspiration cytology (FNAC) reported it as follicular adenoma. Hence, she was planned for a right hemithyroidectomy.
Technique
The patient position is similar to that adopted for standard thyroid surgery. The procedure was performed with the patient in a supine position under general anesthesia with endotracheal intubation. The neck was kept extended, maintaining the chin in the midline. The landmarks were marked initially and the planned site of incision along the skin crease was marked. A central skin incision was made about 3.5 cm long and 3 cm above the sternal notch. The platysma was also incised in the same line and the bleeding points were secured using bipolar diathermy. Upper and lower platysmo-cutaneous flaps were then raised as in conventional thyroidectomy in order to expose the investing layer of deep cervical fascia. The midline was then located by identifying the cervical linea alba which was then incised vertically to about 4-5 cm. A tent-like operative space was thus created and maintained by means of external retraction using small right-angled retractors and no gas insufflation was utilized [Figure 1].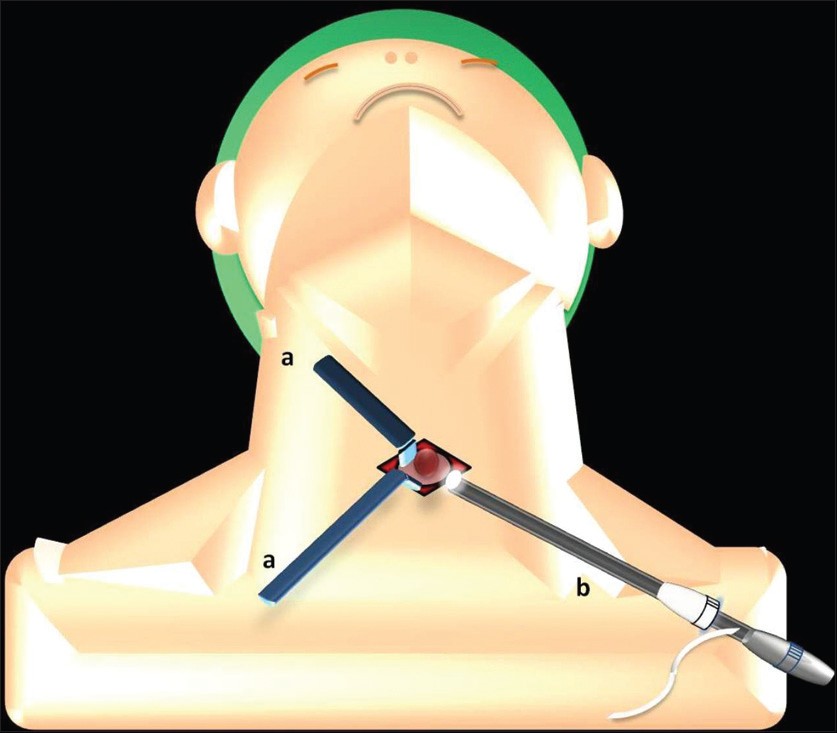 | Figure 1: Schematic representation of GVAT; the surgical field is created by retractors (a) and surgery is performed by the view from the telescope (b)
Click here to view |
The rest of the steps were performed under endoscopic vision using a 5-mm, 30° rigid telescope. With the help of a small Babcock's forceps, the strap muscles were raised and separated from the surface of the gland and then retracted with a small ENT spatula. The dissection was directed to the superior pedicle which was secured and divided between 3-0 absorbable sutures [Figure 2]. The lateral compartment was then exposed and the blunt dissection was carried out separating the loose areolar tissue until the superior and inferior parathyroids could be easily identified [Figure 3]. The dissection was facilitated using a fine non-toothed forceps, a right-angled forceps, a small ENT spatula, and a fine-tipped bipolar diathermy. The recurrent laryngeal nerve was also easily identified at this stage and protected [Figure 4]. The inferior thyroid veins were secured close to the lower pole of the thyroid lobe using only bipolar diathermy. The right lobe was then delivered out of the wound and the gland was divided at the medial border of the left lobe to include the isthmus (right lobectomy with isthmectomy). A suction drain was left in situ. The wound was closed in layers. The operating time was 130 min and blood loss was minimal. The postoperative period was uneventful. The histopathology report was follicular carcinoma. Hence, a completion thyroidectomy was done by the conventional open technique.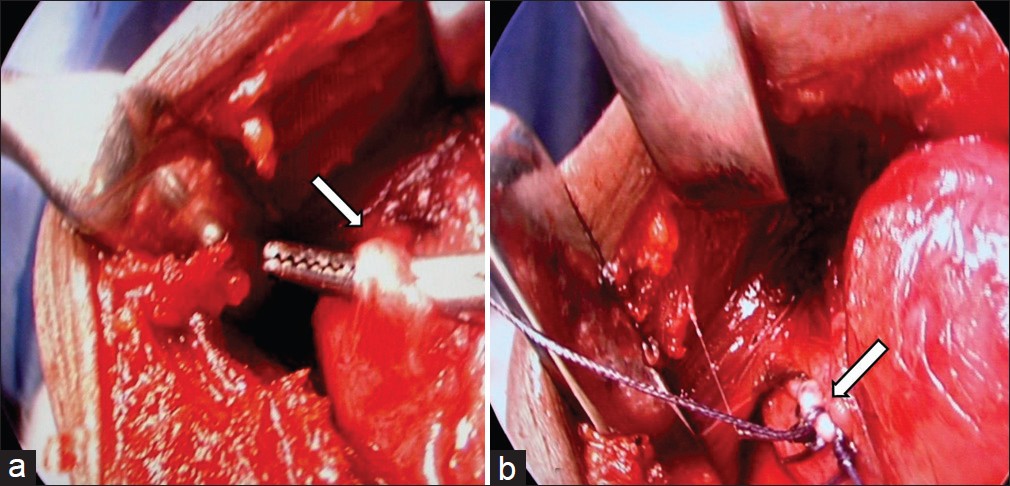 | Figure 2: The superior pedicle seen under magnification (a) and secured with sutures (b)
Click here to view |
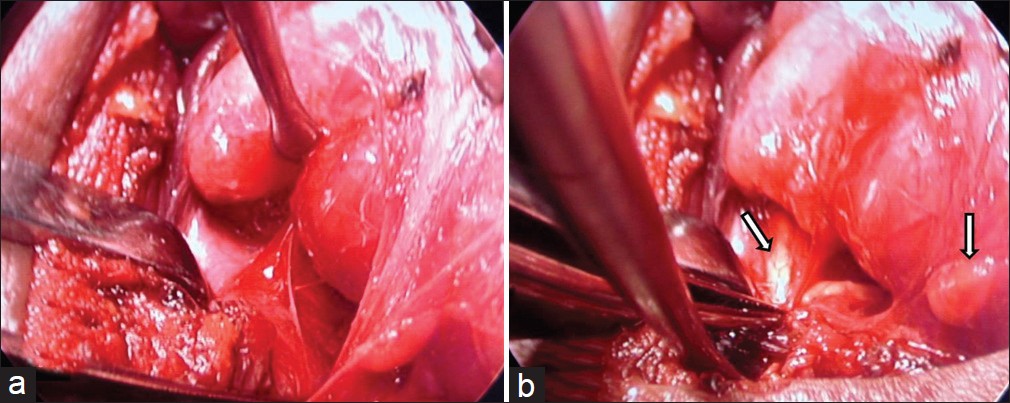 | Figure 3: (a) Endoscopic view of dissection in the lateral compartment. (b) The endoscope provides a magnified view of the parathyroids (white arrows)
Click here to view |
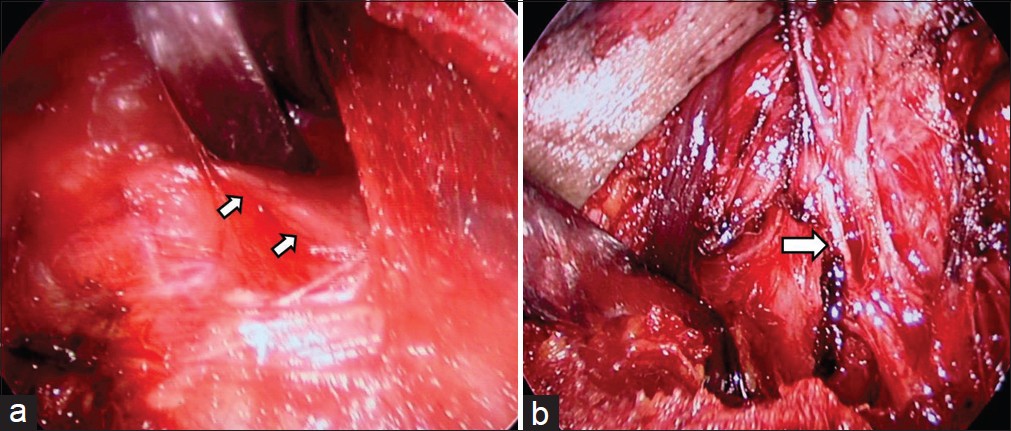 | Figure 4: The recurrent laryngeal nerve (white arrows) is seen during dissection (a) and after removal of the gland (b)
Click here to view |
 Discussion Discussion | |  |
In this modern era of "minimal access surgery," the trend is toward developing surgical procedures that require significantly smaller incisions, with an attempt to reduce pain, shorten the length of hospital stay, and particularly improve cosmesis. Until recently, surgery for the thyroid gland had been known only by one name, i.e. thyroidectomy. This surgery was pioneered by Kocher in 1909, and from then on had been universally accepted as the only available and acceptable technique for thyroid surgery.
Although minimally invasive surgery was fast imbibed into various surgical specialties, it failed to gain such momentum in the field of head and neck surgery, probably owing to anticipated difficulties in the technique and the complex anatomy involved and the concerns of obtaining adequate working space within the limited confines of the neck, all of which are technically challenging. Nevertheless, innovators have enthusiastically developed various minimally invasive thyroid surgical techniques and have shown them to be safe and feasible.
All of this probably started with Gagner's first report describing endoscopic subtotal parathyroidectomy for hyperparathyroidism in 1996. [2] In 1997, Huscher and colleagues first described the complete endoscopic right thyroid lobectomy. Since then, several minimally invasive approaches to thyroid gland have been described. [3]
These procedures have been assigned various terminologies such as MIVAT, minimal access thyroid surgery (MATS), and video-assisted thyroidectomy (VAT). There are essentially three types of approaches, namely, totally endoscopic approach, endoscopically assisted approach, and non-endoscopic minimally invasive thyroid surgery (minimally invasive open thyroidectomy).
Totally endoscopic techniques
In purely endoscopic techniques, the thyroid compartment is approached through various other routes with the help of endoscopes with or without carbon dioxide gas insufflation. Various techniques described include the lateral neck, axillary, anterior chest, and breast approaches. The idea is to entirely avoid scarring the neck. [4],[5],[6]
Endoscopically assisted techniques
MIVAT is the most widely used technique. It was introduced, popularized, and perfected by Miccoli in Italy in the late 1990s. The Miccoli's MIVAT technique utilizes a very small incision (1.5 cm). The dissection is performed utilizing certain special instruments, and ultrasonic shears are used for vascular control. Shimizu's technique (based on the Nagai method for the abdomen), a modification of MIVAT technique, is the video-assisted neck surgery where an anterior neck flap is lifted without using gas insufflation and a tent-like working space is created using a special retraction technique. [7],[8]
Non-endoscopic techniques
Minimally invasive open surgery techniques are also known as "small incision thyroidectomy" and do not require specialized instruments like endoscopes and video assistance. Ottavio et al. described a minimally invasive non-endoscopic technique for thyroidectomy using incisions of 2.5-3 cm. [9]
The procedure described here is inspired by Miccoli's MIVAT technique. Here, superior and inferior musculo-cutaneous flaps are raised to provide maximum working space for the limited incision and working space is produced and maintained by external manual retraction. The remaining procedure reproduces the various operative steps of the standard thyroidectomy. It can be thus considered as a direct "flow on" from the traditional surgery. Moreover, the superior pedicle can be easily accessed and secured by suture ligation, obviating the need for ultrasonic shears which can be considered to be cost effective. In various minimally invasive thyroid procedures, the strap muscles are frequently divided to facilitate adequate exposure of the lobe. In this case, the strap muscles were not divided. This was probably owing to the fact that the strap muscles in this patient were not bulky. In the standard thyroidectomy, a larger incision is required for visualization of the lateral compartment of the thyroid by the unaided eye. While in VAT, the endoscope allows a better and magnified view of these areas, thereby obviating the need for larger incision to facilitate better visual exposure. The recurrent laryngeal nerve and the parathyroids can be easily identified due to the excellent magnification of the endoscope. Moreover, the disadvantages of gas insufflation such as subcutaneous emphysema and hypercarbia can be avoided.
After having successfully performed this procedure, we felt that it would have been probably possible to perform the entire procedure through a smaller incision. In this case, the incision was about 3.5 cm. However this was much smaller than the incision we routinely used for traditional thyroid surgery [Figure 5]. Since this was the first case, we had opted to have a more liberal incision. Logically too, it was considered safer to try performing a hemithyroidectomy as the first case before venturing to perform total thyroidectomy. Patient selection is another important criterion. Most groups advocate minimally invasive thyroid surgeries for a nodule diameter that is less than 30 mm and a thyroid volume below 30 ml. A history of thyroiditis, previous open surgery, and nodules larger than 35 mm are considered the relative contraindications. In this case, the patient was selected for this procedure due to the following reasons: the thyroid nodule was less than 3 cm, a solitary nodule (warranting a hemithyroidectomy), absence of thyroiditis and multinodular change, absence of previous neck surgery, and absence of other comorbidities.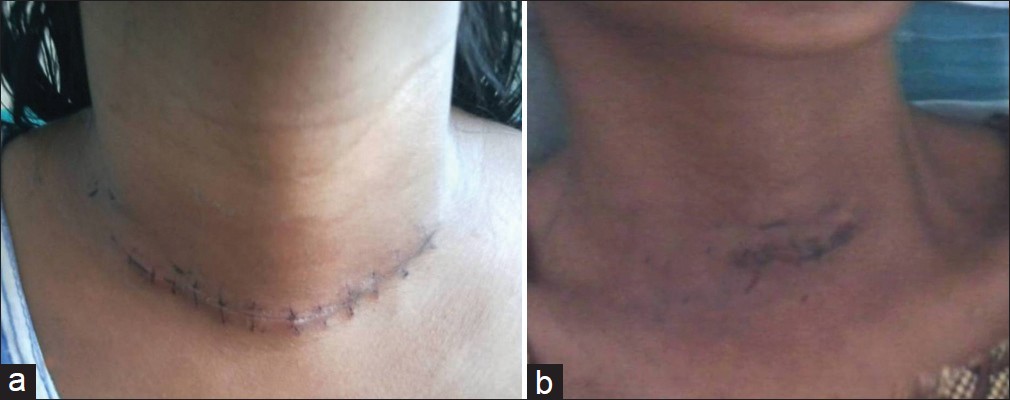 | Figure 5: The size of the incision for GVAT (b) is much smaller than that of our standard thyroidectomy (a)
Click here to view |
The technique described here [gas-less video-assisted thyroidectomy (GVAT)] can be probably employed as an initial training procedure to start performing minimally invasive thyroid surgery and then progressively graduate to performing more minimally invasive procedures such as Miccoli's MIVAT and purely endoscopic thyroidectomies. With experience, the size of the incisions can probably be reduced progressively. The surgeon can also perhaps avoid raising skin flaps and gain direct access to the thyroid compartment from beneath the strernomastoid.
It should also be noted that this case was attempted by the surgeon after having a vast experience of performing open thyroid surgeries. It is therefore felt that surgeons who are well versed with open thyroidectomy can try performing this procedure. In case of any difficulty, it can always be converted to the standard procedure by just extending the incision. In this case, the size of the incision was larger than in various series of minimally invasive techniques described. It is therefore felt that this procedure can be considered as an intermediate or learning procedure to perform MIVAT through smaller incisions (1.5-2 cm). The noted advantages of the present technique are outlined in [Table 1].
The various disadvantages with MITS include the longer duration of surgery, steep learning curve, and increased cost of surgery due to equipment usage. The reported rates of important complications, like recurrent laryngeal nerve palsy and hypoparathyroidism, are similar to those seen after conventional thyroid surgery. Miccoli et al. reported the rates of recurrent nerve palsy and hypoparathyroidism to be 1.3% and 0.3%, respectively, with MIVAT. [10]
Since there is no gold standard procedure for minimally invasive thyroidectomy, it is still not clear as to what size of incision constitutes a minimal access thyroidectomy. If the Kocher's cervicotomy constitutes the conventional access procedure, then it should mean that the term "minimal access thyroidectomy" should apply to all procedures that are performed through smaller access incisions. The general consensus is that a skin incision less than 6 cm is considered minimally invasive, although others have proposed that the term minimal access thyroidectomy should be reserved for incisions shorter than 3.0 cm. [11],[12] In a study comparing scar aesthetics in minimal access parathyroidectomy versus conventional thyroidectomy, it was shown that the larger scars of conventional surgery were more conspicuous to the naïve viewers, but there was no decrease in patient satisfaction. [13]
In this case, the completion thyroidectomy was done by the conventional or open technique, as for now, completion thyroidectomy by the conventional technique is recommended for thyroid carcinoma until further evidence is available. [14]
 Conclusion Conclusion | |  |
Endoscopic thyroid surgery is still in its evolving phase. Although there is no accepted gold standard procedure for minimally invasive thyroid surgery, the incision made during video-assisted surgery is much smaller than that used for traditional surgery. The procedure described here can be considered as a more cost-effective alternative to the conventional MIVAT, and therefore is feasible in rural settings and can be performed by surgeons who are already well versed with open thyroid surgeries. This technique can also serve as a learning tool to perform much more minimally invasive thyroidectomies. Further research is needed to assess the true potential of the technique.
 References References | |  |
| 1. | Miccoli P, Berti P, Conte M, Bendinelli C, Marcocci C. Minimally invasive surgery for small thyroid nodules: Preliminary report. J Endocrinol Invest 1999;22:849-51. 
[PUBMED] |
| 2. | Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 1996;83:875. 
[PUBMED] |
| 3. | Hüscher CS, Chiodini S, Napolitano C, Recher A. Endoscopic right thyroid lobectomy. Surg Endosc 1997;11:877. 
|
| 4. | Ikeda Y, Takami H, Sasaki Y, Kan S, Niimi M. Endoscopic neck surgery by the axillary approach. J Am Coll Surg 2000;191:336-40. 
|
| 5. | Takami H, Ikeda Y. Minimally invasive thyroidectomy. ANZ J Surg 2002;72:841-2. 
|
| 6. | Ohgami M, Ishii S, Arisawa Y, Ohmori T, Noga K, Furukawa T, et al. Scarless endoscopic thyroidectomy: Breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 2000;10:1-4. 
|
| 7. | Shimizu K, Kitagawa W, Akasu H, Hatori N, Hirai K, Tanaka S. Video-assisted endoscopic thyroid and parathyroid surgery using a gasless method of anterior neck skin lifting: A review of 130 cases. Surg Today 2002;32:862-8. 
|
| 8. | Ohki J, Nagai H, Hyodo M, Nagashima T. Hand-assisted laparoscopic distal gastrectomy with abdominal wall-lift method. Surg Endosc 1999;13:1148-50. 
|
| 9. | Cavicchi O, Piccin O, Ceroni AR, Caliceti U. Minimally invasive non-endoscopic thyroidectomy. Otolaryngol Head Neck Surg 2006;135:744-7. 
|
| 10. | Miccoli P, Berti P, Raffaeli M, Materazzi G, Baldacci S, Rossi G. Comparison between minimally invasive video assisted thyroidectomy and conventional thyroidectomy: A prospective randomized study. Surgery 2001;130:1039-43. 
|
| 11. | Brunaud L, Zarnegar R, Wada N, Ituarte P, Clarke OH, Duh QY. Incision length for standard thyroidectomy and parathyroidectomy: When is it minimally invasive? Arch Surg 2003;138:1140-3. 
|
| 12. | Ruggieri M, Straniero A, Genderini M, D'Armiento M, Fumarola A, Trimboli P, et al. The size criteria in minimally invasive video-assisted thyroidectomy. BMC Surg 2007;7:2. 
|
| 13. | O'Connell DA, Diamond C, Seikaly H, Harris JR. Objective and subjective scar aesthetics in minimal access vs conventional access parathyroidectomy and thyroidectomy surgical procedures: A paired cohort study. Arch Otolaryngol Head Neck Surg 2008;134:85-93. 
|
| 14. | Gagner M, Inabnet WB 3rd. Endoscopic thyroidectomy for solitary thyroid nodules. Thyroid 2001;11:161-3. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
[Table 1]
|