|


 |
| SURGICAL TECHNIQUE |
|
| Year : 2012 | Volume
: 4
| Issue : 2 | Page : 89-91 |
|
|
Mesh-free Ventral Rectopexy for Women with Complete Rectal and Uterovaginal Prolapse
Adedayo O Tade1, Adetola O Olatunji2
1 Department of Surgery, Olabisi Onabanjo University Teaching Hospital, Sagamu, Nigeria
2 Department of Obstetrics and Gynecology, Olabisi Onabanjo University Teaching Hospital, Sagamu, Nigeria
| Date of Web Publication | 8-Apr-2013 |
Correspondence Address:
Adedayo O Tade
Department of Surgery, Olabisi Onabanjo University Teaching Hospital, Sagamu
Nigeria
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.110256

 Abstract Abstract | | |
Background: Mesh rectopexy may be associated with infective complications, erosion into the vagina or rectum, and disintegration or dislodgement. A mesh-free rectopexy will avoid these complications. Objective of the study was to perform mesh-free ventral rectopexy and assess its safety and effectiveness. Materials and Methods: Nine women with complete rectal and uterovaginal prolapse were treated with total abdominal hysterectomy, closure of the vaginal vault, extirpation of the pouch of Douglas and suture of anterior rectal wall to the posterior vaginal wall (ventral suture rectopexy). The ventral suture rectopexy was achieved by three pairs of interrupted silk sutures, 2.5 cm above each other, and the first pair very close to the pelvic floor. This composite structure (anterior rectal wall and posterior vaginal wall), sits astride the perineal body. Intussusception and subsequent prolapse of the sutured rectum and vaginal wall is prevented. Vaginal vault prolapse was prevented by the suture of each round ligament of the uterus to the corresponding lateral vaginal fornix. No mesh was used. Results: Nine multiparous women aged between 52 and 70 years had the procedure. The mean operative time was 135 minutes (range 110-220). The follow-up period was between 29 months and 7 years. Full continence was restored in all patients within eight weeks of the operation. Bowel habit returned to once daily in four patients and once every other day in the remaining five patients, within thirteen weeks of surgery. One patient had intermittent mucus discharge per rectum for six months. This stopped without a specific treatment. There has been no known recurrence in these nine patients. One patient developed wound infection as a complication. There was no mortality. All the patients are now asymptomatic. Conclusion: Ventral suture rectopexy is a safe and effective treatment for complete rectal prolapse in a selected group of patients. Keywords: Mesh-free, rectal prolapse, uterovaginal prolapse, vaginal vault prolapse, ventral rectopexy
How to cite this article:
Tade AO, Olatunji AO. Mesh-free Ventral Rectopexy for Women with Complete Rectal and Uterovaginal Prolapse. J Surg Tech Case Report 2012;4:89-91 |
How to cite this URL:
Tade AO, Olatunji AO. Mesh-free Ventral Rectopexy for Women with Complete Rectal and Uterovaginal Prolapse. J Surg Tech Case Report [serial online] 2012 [cited 2016 Jun 10];4:89-91. Available from: http://www.jstcr.org/text.asp?2012/4/2/89/110256 |
 Introduction Introduction | |  |
Complete rectal prolapse is an intussusception of the rectum extending beyond the anal canal. It causes considerable discomfort and social embarrassment and is associated with a variety of symptoms including fecal incontinence, constipation and diarrhoea, persistent mucus discharge and bleeding and excoriation of the mucosa of the prolapsed rectum. Abdominal rectopexy is the standard treatment for such patients provided they are fit for the surgery. Dorsal mesh rectopexy after complete rectal mobilization has a recurrence rate of 5%, but it is associated with a poor functional state, usually in the form of induced constipation. [1],[2] Resection mitigates this dysfunction but risks a pelvic anastomosis. Autonomic denervation of the rectum subsequent to its complete mobilization has been suggested as a contributory factor. Ventral mesh rectopexy with limited dissection and preservation of lateral rectal ligaments has been found to be safe and free from the complication of complete rectal mobilization and dorsal mesh rectopexy. [3] The ventral position of the mesh in ventral rectopexy, as well as the sparing the lateral ligaments may explain the beneficial effect on symptoms of obstructed defecation. [1],[2],[3]
Most recent published works now employ ventral mesh rectopexy, either laparoscopically or via laparotomy, with good results. [1],[2],[3] The disadvantage of these procedures (ventral and dorsal mesh rectopexy), which have a low recurrence rate of 5%, is that they involve the use of foreign material. The use of a mesh may however be associated with infective complication, erosion into the vagina or rectum, and disintegration or dislodgement. [4],[5]
The role of the mesh in preventing recurrence of the prolapse has been controversial. While the mesh was expected to induce fibrosis that will cause adhesion of the rectum to the sacrum, the ability of the various meshes to generate enough fibrosis has been questioned. An editorial comment in the 1977 edition of 'Operative Surgery' colon, rectum, and anus, suggested that in Ivalon sponge rectopexy, the Ivalon stops the prolapse by forming a rigid cuff at the bottom of the rectovaginal pouch rather than causing adhesion to the sacrum. [6]
We report a technique of repair of complete rectal prolapse, by suture of anterior rectal wall to the posterior vaginal wall (ventral suture rectopexy). We believe that intussusception, and subsequent rectal prolapse, is stopped by the sutured anterior wall of the rectum and posterior vaginal wall sitting astride the perineal body and staying above the pelvic floor. Essentially this method avoids the need for insertion of foreign material. A search of publications in English Language yielded no report on mesh-free ventral rectopexy.
 Materials and Methods Materials and Methods | |  |
Nine consecutive patients presenting with complete rectal and uterovaginal prolapse were included in the study. Patients, who had hysterectomy or major pelvic surgery prior to presentation, were excluded because the anatomy of the pelvis in these patients might be altered. Also excluded were patients with damaged perineal body. Sphincter tone and voluntary contraction were assessed by the number of fingers accommodated without discomfort and the strength of contraction over the examining fingers. The study was approved by the Ethics Review Committee of the hospital. Informed written consent was signed by all patients prior to enrolment into the study.
Operative technique
All patients receive pre operative enema and antimicrobial prophylaxis. The patient lies supine with 20° head down tilt. The urinary bladder is catheterized. The prolapse is reduced manually. The abdomen is opened through a lower abdominal incision. Total abdominal hysterectomy and bilateral salpingo-oophorectomy is done. Each round ligament of the uterus is sutured to the corresponding lateral vaginal fornix. The vaginal vault is closed with interrupted 2/0 vicryl sutures.
The recto sigmoid junction is retracted to the left, the peritoneum is incised over the sacral promontory, and extended along the side of the mesorectum and continued in front of the Pouch of Douglas. The rectovaginal septum is opened and freed as far as possible to the pelvic floor. Traction on the rectum reduces the intussusception. The peritoneal sac in the pouch of Douglas is excised. No posterior or lateral rectal ligament dissection is carried out. The anterior rectal wall (seromuscular layer only) is sutured to the post vaginal wall (seromuscular layer only) by 3 pairs of sutures (silk 2/0), one pair 2.5 cm above the other, and the first as close as possible to the pelvic floor. The pelvic peritoneum is closed above the vaginal vault, thereby extirpation the pouch of Douglas. No mesh is used. The abdomen is closed in the routine manner with no drainage of the pelvic cavity.
Post-operative care
Patient continues on nil by mouth and intravenous fluids until bowel sounds return. Fluid diet followed by regular diet is then allowed. Antimicrobials are administered intravenously for 48 hours. Skin stitches are removed 7-10 days post operation.
Follow-up
Patients were seen in the surgical outpatients fortnightly for first two visits after discharge from hospital, then monthly for six months, thereafter every six months. They were however advised to report to the hospital in the event of any complaint. At each visit, enquiries were made concerning prolapse and bowel habit. Digital rectal examination was done to assess sphincter tone and power of voluntary contraction.
 Results Results | |  |
Nine women with complete rectal and uterovaginal prolapse were treated between January 1998 and December 2007. Their ages (in years) were 52, 53, 53, 56, 59, 62, 63, 68, and 70. The parity of the women was between 6-11 children. The duration of prolapse varied from four to nine years (mean 6.3 years). Other symptoms are shown in [Table 1]. The mean operating time was 135 minutes (range 110-220). Duration of hospital stay was 10-16 days (mean 12.2). Follow-up period was 29 months to 7 years. There was no mortality. Full continence was restored in all patients within eight weeks of the operation. Bowel habit returned to once daily in four patients and once every other day in the remaining five patients, within thirteen weeks of surgery. One patient had intermittent mucus discharge per rectum for six months. This stopped without a specific treatment. No cause for the mucus discharge was found. There has been no known recurrence in these nine patients. The functional results are summarized in [Table 1].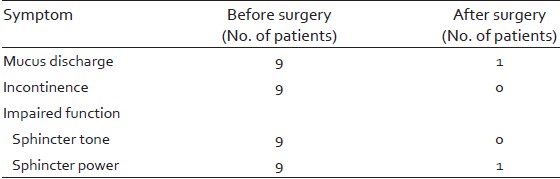 | Table 1: Clinical results of ventral suture rectopexy in nine women with complete rectal prolapse
Click here to view |
 Discussion Discussion | |  |
Full thickness rectal prolapse is an intussusception of the rectum extending beyond the anal canal, occurring mainly in elderly and parous women. The vaginal support system includes apical support provided by the cardinal-uterosacral complex, and lateral support, provided by pubocervical and rectovaginal fascia. Relaxation of this support system is seen with childbirth and ageing. Complete rectal prolapse is uncommon in our environment. [7],[8],[9] It occurs mainly in elderly and multiparous women in whom there is usually an associated uterovaginal prolapse. In this study, all nine patients were elderly multiparous women, the youngest patient was 52 years old, the lowest parity was 6, and one patient had 11 children.
This technique of ventral suture rectopexy is simple and easy to achieve. The rectum and vagina already lie in close apposition such that suturing of the anterior rectal wall to the posterior vaginal wall is tension free. The tissues hold sutures well with little risk of sutures cutting through. Rectal intussusception and subsequent prolapse is prevented by the attachment of the rectum to the posterior vaginal wall. Sliding of the rectum and vagina through the pelvic floor is prevented by the perineal body since they sit astride the perineal body, the rectum passing downwards and backwards behind the perineal body, while the vagina continues downwards and forward in front of the perineal body. Closure of the vault of the vagina and suture of the round ligament of the uterus to the corresponding lateral vaginal fornix contributes to the prevention of vaginal vault prolapse.
Open technique (laparotomy) was employed because facilities for laparoscopic technique were not available in our centre. Laparoscopic ventral suture rectopexy is certainly feasible where facilities and expertise exist.
Functional results are shown in [Table 1]. The minimum follow up period was 29 months. During this period no recurrence occurred. Full continence was regained within 8 weeks of the surgery, while bowel habit returned to once daily or once every other day, within thirteen weeks of surgery. One patient had intermittent mucus discharge per rectum for six months. This stopped without a specific treatment. No cause was found. These results are comparable to those from ventral mesh rectopexy [1],[2],[3] but without the risk of complications associated with insertion of a foreign body, the mesh. [4],[5]
The limitation of this study was the small number of suitable patients; only nine patients were recruited in ten years. This is partly because rectal prolapse in uncommon in our environment. [7],[8],[9]
 Conclusion Conclusion | |  |
In conclusion, ventral suture rectopexy is a safe and effective treatment for complete rectal prolapse in a selected group of patients.
 References References | |  |
| 1. | D' Hoore A, Cadoni R, Penninckx F. Long term outcome of laparoscopic ventral rectopexy for total rectal prolapse. Br J Surg 2004; 91:1500-5. 
|
| 2. | Portier G, lovino F, Lazorthes F. Surgery for rectal prolapse: Orr-loygue ventral, rectopexy with limited dissection prevents post operative - induced constipation without increasing recurrence. Dis Colon Rectum 2006;49:1136-40. 
|
| 3. | Boons P, Collinson R, Cunningham C, Lindsey I. Laparoscopic ventral rectopexy for external rectal prolapse improve constipation and avoid de novo constipation. Colorectal Dis 2010;12:526-32. 
|
| 4. | Karagulle E, Yildirim E, Turk E, Akkaya D, Moray G. Mesh invasion of the rectum: An unusual late complication of rectal prolapse repair. Int J Colorectal Dis 2006;21:724-7. 
|
| 5. | Chen RW, Musser AW, Postlethwaithe RW. Alterations of and tissue reactions to polyvinyl alcohol sponge implants. Surgery 1969;66:899-906. 
|
| 6. | Nigel H. Porter. Complete rectal prolapse: Ivalon sponge repair. In: Todd IP, editor. Operative surgery fundamental international techniques colon rectum anus. London: Butterworths; 1977. p. 220-4. 
|
| 7. | Nwabunike TO, Ojukwu JO. Complete rectal prolapse in Enugu, Nigeria. Scand J Gastroenterol Suppl 1986;124:179-82. 
|
| 8. | Akinola DO, Agbakwuru EA. Management of rectal prolapse in Ile- Ife, Nigeria. East Afr Med J 1991;68:795-800. 
|
| 9. | Adisa AC, Mbanaso AU. Simple abdominal rectopexy for complete rectal prolapse. J Med Invest Pract 2001;2:23-5. 
|
[Table 1]
|