|


 |
| ORIGINAL ARTICLE |
|
| Year : 2013 | Volume
: 5
| Issue : 1 | Page : 13-17 |
|
|
Laparoscopic inguinal hernia repair in a developing nation: Short-term outcomes in 103 consecutive procedures
Shamir O Cawich1, Sanjib K Mohanty2, Kimon O Bonadie1, Lindberg K Simpson1, Peter B Johnson1, Sundeep Shah1, Eric W Williams1
1 Department of Surgery, University of the West Indies, Mona, Kingston 7, Jamaica, West Indies
2 Department of Surgery, Cayman Islands Hospital, Grand Cayman, British, British West Indies
| Date of Web Publication | 21-Sep-2013 |
Correspondence Address:
Shamir O Cawich
Department of Surgery, University of the West Indies, Mona, Kingston 7, Jamaica,
West Indies
 Source of Support: None, Conflict of Interest: None  | 1 |
DOI: 10.4103/2006-8808.118601

 Abstract Abstract | | |
Background: There are no published data on the outcomes of inguinal hernia repair from the Anglophone Caribbean. To the best of our knowledge, this is the first report of a series of laparoscopic inguinal hernia repairs from the region. Materials and Methods: Data was extracted from a prospectively maintained database of consecutive trans abdominal pre-peritoneal (TAPP) repairs done between June 1, 2005 and May 30, 2012. Perioperative data collected included patient demographics, hernia type, operative technique, duration of surgery, intra-operative details, morbidity, analgesia requirements, and duration of hospitalization. A telephone survey was also performed to identify late recurrences and complications. Descriptive statistics were generated using Statistical Package for Social Sciences (SPSS) Ver 12.0. Results: There were 103 consecutive TAPP procedures in 88 patients at an average age of 35.4 years ± 12.9 (standard deviation; SD) and average body mass index (BMI) of 28.9 Kg/m 2 ± 2.23 (SD). The indications were bilateral (30), recurrent unilateral (24), and primary unilateral (49) inguinal hernias. The mean duration of operation was 68.5 minutes (SD ± 10.4; Range: 55-95; Median 65; Mode 65) minutes for unilateral TAPP and 89 minutes (SD ± 7.61; Range: 80-105; Median 90; Mode 90) for bilateral repairs. Post-operatively, 65/70 patients required ≤1 dose of parenteral opioid analgesia and 74 (84.1%) patients discontinued oral analgesia within 48 hours of operation. Complications were recorded in six (5.8%) cases and a recurrence in one (0.97%) case after a mean follow-up period of 3.2 years (SD ± 1.8; Range: 0.5-7). Conclusion: Laparoscopic inguinal hernia repair is a safe and effective operation in this setting. Keywords: Hernia, laparoscopic, recurrence, TAPP
How to cite this article:
Cawich SO, Mohanty SK, Bonadie KO, Simpson LK, Johnson PB, Shah S, Williams EW. Laparoscopic inguinal hernia repair in a developing nation: Short-term outcomes in 103 consecutive procedures. J Surg Tech Case Report 2013;5:13-7 |
How to cite this URL:
Cawich SO, Mohanty SK, Bonadie KO, Simpson LK, Johnson PB, Shah S, Williams EW. Laparoscopic inguinal hernia repair in a developing nation: Short-term outcomes in 103 consecutive procedures. J Surg Tech Case Report [serial online] 2013 [cited 2016 May 25];5:13-7. Available from: http://www.jstcr.org/text.asp?2013/5/1/13/118601 |
 Introduction Introduction | |  |
Laparoscopic inguinal hernia repair has become commonplace since the first descriptions in the early 1990s. [1],[2],[3] For selected indications (obesity, bilateral hernias, and recurrent hernias), there are data demonstrating an advantage to laparoscopic inguinal hernia repair with improved post-operative pain profiles, [4],[5],[6],[7],[8],[9] earlier return to work, [6],[7],[8],[9],[10],[11] quicker resumption of normal activity, [5],[7],[8],[10],[11] and reduced incidence of chronic groin pain/numbness. [12],[13]
However, the techniques have not been fully embraced by the Caribbean surgical community, probably because there is a requirement for increased training and a steep learning curve. A literature review in Medscape, Medline, Pubmed, Embase, and Scilo performed in January 2013 returned no reports of laparoscopic inguinal hernia repair from the Anglophone Caribbean. To the best of our knowledge, this is the first report of a series of laparoscopic inguinal hernia repairs from the region.
 Materials and Methods Materials and Methods | |  |
A database of all laparoscopic inguinal hernia repairs involving the authors was maintained from June 1, 2005. The database was accessed to identify all consecutive patients who had laparoscopic inguinal hernia repairs performed between June 1, 2005 and May 30, 2012. Their hospital records were retrieved and the following data collected: Patient demographics, body mass index (BMI), hernia type, operative details, morbidity and hospitalization. The retrospective methodology did not allow the use of pain assessment scores, so the number of doses of parenteral analgesia administered was used as a proxy for post-operative pain.
We performed a telephone survey to identify late complications or recurrences. A recurrence was defined as a clinically detectable ipsilateral groin swelling with a cough impulse. Patients, who reported symptoms suggestive of a recurrence, were asked to return for clinical review at the specialist clinics. Descriptive statistics were generated using Statistical Package for Social Sciences (SPSS) Ver 12.0.
Although, there was minor variation in peritoneal access and port placement, the operative techniques were relatively standard. Prophylactic antibiotics were not routinely administered. The patients were positioned on the operating table with arms tucked by the sides in a 20° Trendelenburg position and monitors near the feet. A visual port was inserted at the umbilicus and two working ports at the mid-clavicular line approximately 2 cm cephalad to the umbilicus on either side of the midline.
We used a trans-abdominal pre-peritoneal (TAPP) approach that commenced with a transverse peritoneal incision 3 cm above the deep ring, extending from the medial umbilical ligament to the anterior superior iliac spine. The peritoneal incision was used to develop a peritoneal flap inferiorly [Figure 1]. The hernial sac was separated from cord structures until it was fully reduced. For large inguino-scrotal hernias, the sac was transected at the deep ring and allowed to remain in situ [Figure 2]. The dissection was similar for bilateral herniae and converged at the symphysis.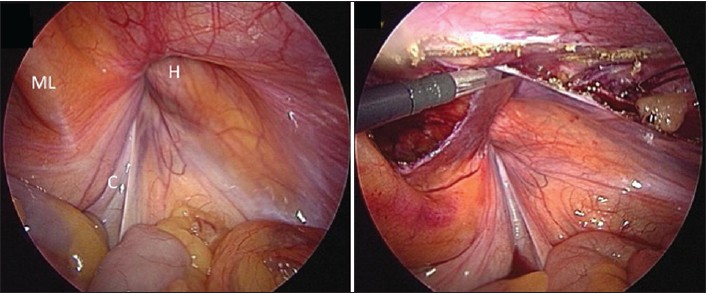 | Figure 1: Peritoneal flap being developed using a transverse peritoneal incision placed above the hernial orifice (h); ML = Medial umbilical ligament; C = cord structures
Click here to view |
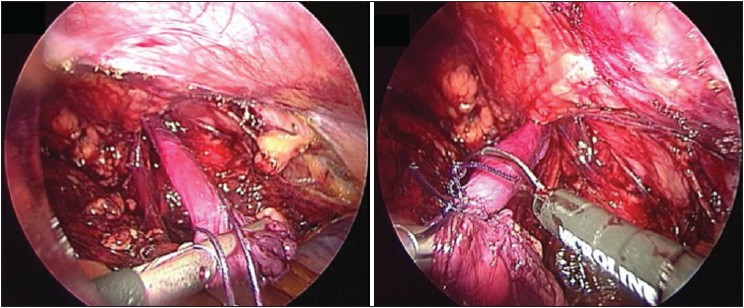 | Figure 2: Hernia sac separated from cord structures, ligated and transected, allowing sac to remain in situ without dissection into the scrotum
Click here to view |
Once the pre-peritoneal space was prepared, a 15 × 15 cm lightweight polyester mesh (Parietex® , Covidien Inc, Mansfield, MA) was positioned to cover the hernia orifice [Figure 3]. The mesh was fixated to pubic ramus and Cooper's ligament with endoscopic tackers (Protack® , Covidien Inc, Mansfield, MA). The superior margins of the mesh were then fixated to the abdominal wall, deliberately avoiding the inferior epigastric vessels. No fixation was used infero-laterally. After satisfactory mesh placement, the peritoneal opening was then closed [Figure 4].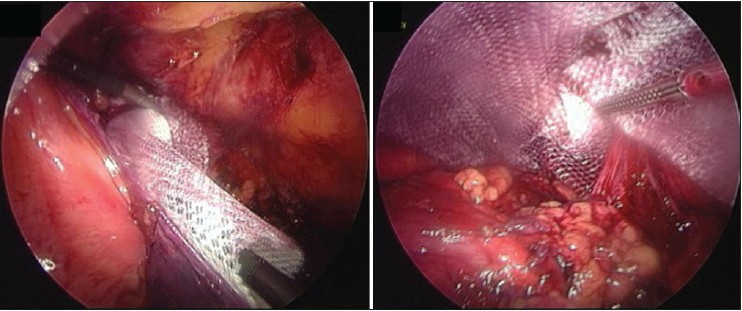 | Figure 3: Lightweight polyester mesh introduced into the pre‑peritoneal pocket, positioned over the hernial orifices and fixated with endoscopic tackers starting at the retropubic space of Retzius
Click here to view |
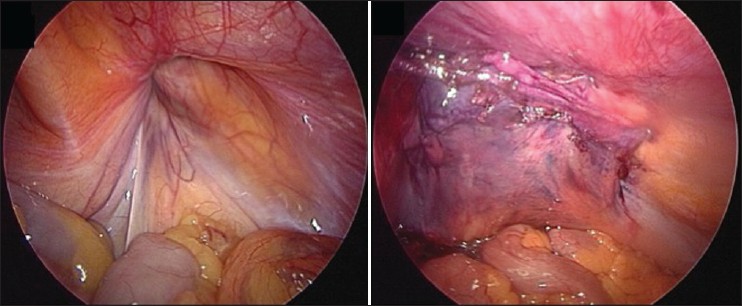 | Figure 4: Laparoscopic view of right inguinal region pre and post laparoscopic TAPP repair
Click here to view |
Post-operatively, the patients were encouraged to ambulate and have normal diet. Oral analgesia was routinely administered, with parenteral opioids on demand only. The patients were discharged once they tolerated diet and were pain-free. We encouraged patients to return to normal activity and exercise immediately after hernia repair.
In an attempt to examine our learning curve, we divided the data into two equal periods: An early period from June 1, 2005 to December 31, 2008 and a late period from January 1, 2009 to May 30, 2012. We compared morbidity, recurrence, and operative time as the main outcome measures in these two groups. The Student's t-test was used to compare the end points for each of the two periods. A P < 0.01 was considered significant.
 Results Results | |  |
Over the study period, 88 patients had laparoscopic inguinal hernia repair by one of two surgeons. There were nine females and 79 males at an average age of 35.4 years ± 12.9 (standard deviation; SD) and average BMI of 28.9 Kg/m 2 ± 2.23 (SD). The indications were bilateral hernias (30), recurrent unilateral hernias (24), and primary unilateral hernias (49). There was an additional operative procedure performed at the same sitting in 18 cases.
We considered each hernia repair as a separate procedure since each repair carried its own risk of complications and recurrence. Therefore, we counted the number of procedures (laparoscopic hernia repairs) performed. There were 15 patients with bilateral hernias who had laparoscopic repairs on both sides, totaling 30 repairs. Each of the remaining 73 patients (49 primary unilateral and 24 recurrent unilateral) had one procedure done. In total, there were 103 laparoscopic inguinal hernia repairs in this study.
The mean duration of operation for patients who had hernia repair only was 68.5 minutes (SD ± 10.4; Range: 55-95; Median 65; Mode 65) for unilateral repairs and 89 minutes (SD ± 7.61; Range: 80-105; Median 90; Mode 90) for bilateral repairs.
For the patients who only had TAPP repair, 51/70 required no parenteral opioid analgesia after operation. A single dose of parenteral opioid analgesia was administered to 14 patients and five patients required >2 doses. After discharge, 12/70 (17.1%) patients required no oral analgesia and 62/70 (88.6%) patients stopped their oral analgesia within 48 hours. Only eight patients required oral analgesia for >48 hours.
There were early complications recorded in six (5.8%) cases as outlined in [Table 1]. A telephone interview was conducted to identify late complications. None of the patients reported chronic groin pain or numbness but one patient reported a swelling at the ipsilateral groin and was asked to come for specialist review. This was the only recurrence (0.97%) in this series. This recurrence occurred within a year in a patient who could not afford to purchase lightweight mesh. In this case, we decided to proceed with Prolene® mesh (Ethicon, Aurangabad, India) but found it difficult to handle and seat properly with laparoscopic instruments.
Analyzing the data across the study groups, 42 repairs were performed in the early period. In this period, hernia repairs were performed in a mean operating time of 71.06 ± 9.82 minutes (Range: 60-95), with a complication reported in four (9.5%) cases and one recurrence (2.4%). There were 61 repairs performed in the late period with a mean operating time of 64.96 ± 10.21 minutes (Range: 55-85), a complication in two (3.3%) cases, and no recurrences. While there was a downward trend in all values, there was no demonstrable statistical difference in operating time (P = 0.03), morbidity (P = 0.15) or recurrence (P = 0.21) between the two periods.
 Discussion Discussion | |  |
The first laparoscopic inguinal hernia repair was described in 1990 by Ger et al., [1] and involved simply covering the internal defect with an intra-peritoneal mesh. Currently, the accepted modern techniques for inguinal hernia repair are the TAPP and totally extra-peritoneal (TEP) repairs.
Arregui et al., [2] described the TAPP approach in 1992 that requires intra-peritoneal access to position mesh in a pre-peritoneal space. McKernan et al., [3] described the TEP technique in 1993, where mesh is placed in a similar position without breaching peritoneum. A practice survey of 100 laparoscopic surgeons participating in the 2010 Congress of the European Association of Endoscopic Surgeons revealed that TAPP was the most commonly used technique for laparoscopic inguinal hernia repair. [14] We also used the TAPP technique as we found it technically simpler with better anatomic detail. Additionally, pre-peritoneal balloon dissectors were not routinely available in our setting. [15],[16],[17]
Despite the existence of data to prove that laparoscopic inguinal hernia repair has advantages over open repair for selected indications, surgeons in the Anglophone Caribbean have not embraced the laparoscopic techniques. A survey of practicing surgeons in Jamaica at the 2012 Association of Surgeons' Annual Conference [16] revealed a reluctance to use laparoscopy because it was more expensive than open repair. Many surgeons also pointed to the fact that public facilities in Jamaica do not stock lightweight mesh or fixation devices for use in these procedures. The patient desirous of laparoscopic repair in this setting would independently have to source any disposables required to complete their operation.
The scarcity of surgical disposables and laparoscopic supplies in public facilities is a recognized obstacle to the advancement of laparoscopic surgery in Jamaica [16],[17] and across the Caribbean. [15] We may be able to overcome this by relying more on intra-corporeal suturing instead of commercial tackers and/or staplers. Otherwise, the basic instrumentation for TAPP repair is the same as that for cholecystectomy that is already done extensively in this setting. [15]
Community surgeons also voiced concern that the techniques had not been validated in the local setting. [16] Unfortunately, there are no published data on open inguinal hernia repair from any country in the Caribbean with which we can compare our results. However, the study revealed that TAPP repairs were being performed in this setting with good outcomes, similar to that seen in international medical literature.
The time to complete a TAPP repair in this series (68.5 minutes for unilateral; 89 minutes for bilateral) compared well with results from larger series where the mean operative time ranged from 25 minutes [18] to 102 minutes [19] for unilateral TAPP and 38 minutes [18] to 123 minutes [19] for bilateral TAPP repairs.
Overall morbidity in this series (5.8%) also compared well with overall morbidity in existing reports of TAPP repairs that range from 8% [20] to 20% [19] of cases. We had one iatrogenic sigmoid injury that may not have occurred with open repair, but the argument can also be made that it could have been avoided with TEP repair. Therefore, we do not believe that the potential for intra-peritoneal injury can be used as an argument against laparoscopy. On the contrary, it forced us to re-think our position on TEP, and we have been using TEP techniques more frequently, but admittedly less frequently than TAPP repair.
There was one hematoma in a patient with a large inguino-scrotal hernia who had extensive dissection of the sac in an attempt at reduction. Since then, we make no attempt to reduce the sac in large inguinoscrotal hernias. Instead, the sac is transected and left in situ. While this reduced the incidence of scrotal hematoma, it created a new problem because fluid now accumulated in the distal sac. This may be the reason we noticed an increase in the incidence of scrotal seromas in the latter part of our experience. Most of our patients were dissatisfied about this. We now counsel all our patients with large hernia preoperatively, informing them of the risk of seroma formation but reinforcing that the majority resolve spontaneously. Even so, the incidence of scrotal seroma (1.9%) in this series compares favorably with the incidence in larger series that range from 1.06% [21] to 11% [18] of cases.
There was one iatrogenic inferior epigastric artery injury that was controlled with sutures. We later realized that the laparoscope could be used to trans-illuminate the abdominal wall so that we could avoid firing the staples at that point. Since then, we have made this as a deliberate step in the operation.
The only other complication seen in this series was urinary retention (0.97%). As with open hernia repair, this is not an uncommon complication. Urinary retention has been reported in up to 33% [21] of TAPP repairs. In an attempt to limit the incidence, we now mobilize patients early after operation.
One of the advantages of laparoscopic repair is the reduction in post-operative pain. [4],[5],[6],[7],[8],[9] Due to the retrospective nature of this study, we were not able to assess post-operative pain with standardized pain scores but we did use the number of doses of on-demand parenteral opioid analgesia required as a proxy for post-operative pain. The TAPP repair had good pain profiles, with 93% of patients requiring ≤1 dose of parenteral analgesia post-operatively and 88.6% discontinuing their oral analgesia within 48 hours of operation.
Several randomized controlled trials have demonstrated that the recurrence rates are statistically similar after open and laparoscopic repairs. [9],[10],[20],[21] We had a single recurrence (0.97%) that occurred in the second year of our experience with TAPP repairs in a patient in whom we used a piece of regular polypropylene mesh trimmed from a larger sheet. We found this mesh difficult to handle and seat with laparoscopic instruments. Therefore, we now insist on utilizing lightweight polypropylene or polyester mesh for TAPP repairs.
We also try to adhere to the fundamental principle to spend time creating a generous peritoneal pocket to accommodate a 12 × 15 cm mesh sitting flat and covering all areas of anatomic weakness. With routine observation of these principles, our recurrence rates have remained within acceptable standards, quoted in international literature to be between 0% [20] and 4.3% [21] of TAPP repairs.
When the data were analyzed chronologically between the two time periods, there was a downward trend in mean operating time (71.06 vs. 64.96 minutes; P = 0.03), overall morbidity (9.5% vs. 3.3%; P = 0.15), and recurrence (2.4% vs. 0; P = 0.21). Although the small sample size did not allow any of these differences to achieve statistical significance, we believe it is still reflective of the institutional learning curve.
Study limitations
There are several limitations to this study. Although this is the first report of laparoscopic inguinal hernia repairs from the region, it is a retrospective study with relatively small patient numbers. Nevertheless, we believe it is important to analyze these outcomes to have a realistic appreciation for the outcomes of repair in the hands of community surgeons who are performing repairs infrequently.
Although we reported a single recurrence (0.97%), the average duration of post-operative follow up in this series was 3.2 years (SD ± 1.8; Range: 0.5-7). We acknowledge that this is a relatively short period to evaluate recurrence, which we expect to increase with time. Using the formula proposed by Halverson and McVay [22] to predict recurrence 25 years after operation (number of recurrences at 2 years multiplied by 2.5), this series would have an adjusted long-term recurrence rate of 2.4% at 25 years. A long term study is needed before a comment can be made on the recurrence after laparoscopic inguinal hernia repair in this setting.
 Conclusions Conclusions | |  |
The laparoscopic TAPP inguinal hernia repair is a safe operation in this setting. The principles that we have learned in our experience include the use of a generous peritoneal pocket and large mesh, trans-illumination of the abdominal wall to avoid vascular injury.
 References References | |  |
| 1. | Ger R, Monroe K, Duvivier R. Management of indirect inguinal hernias by laparoscopic closure of the neck of the sac. Am J Surg 1990;159:370-3. 
|
| 2. | Arregui ME, Davis CJ, Yucel O. Laparoscopic mesh repair of inguinal hernia using a pre-peritoneal approach: A preliminary report. Surg Laparosc Endosc 1992;2:53-8. 
|
| 3. | McKernan JB, Laws HL. Laparoscopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc 1993;7:26-8. 
[PUBMED] |
| 4. | Wright DM, Kennedy A, Baxter JN. Early outcome after open versus extra peritoneal endoscopic tension-free hernioplasty. Surgery 1996;119:552-7. 
|
| 5. | Wellwood J, Sculpher MJ, Stoker D, Nicholls GJ, Gedds C, Whitehead A, et al. Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: Outcome and cost. BMJ 1998;317:103-10. 
|
| 6. | Millikan KW, Kosik ML, Doolas A. A prospective comparison of transabdominal preperitoneal laparoscopic hernia repair versus traditional open hernia repair in a university setting. Surg Laparosc Endosc 1994;4:247-53. 
[PUBMED] |
| 7. | Stoker DL, Speilgelhalter DJ, Singh R, Wellwood JM. Laparoscopic versus open inguinal hernia repair: Randomised prospective trial. Lancet 1994;343:1243-5. 
|
| 8. | Hamza Y, Gabr E, Hammadi H, Khalil R. Four arm randomized trial comparing laparoscopic and open hernia repairs. Int J Surg 2010;8:25-8. 
[PUBMED] |
| 9. | Dallas KB, Erovlich D, Choi JJ, Rosa JH, Lo C, Colon MJ, et al. Laparoscopic versus open inguinal hernia repair in octogenarians: A follow-up study. Geriatr Gerontol Int 2013;13:329-33. 
|
| 10. | Brooks DC. A prospective comparison of laparoscopic and tension-free open herniorraphy. Arch Surg 1994;129:361-6. 
[PUBMED] |
| 11. | Wilson MS, Deans GT, Brough WA. Prospective trial comparing Lichenstein with laparoscopic tension-free mesh repair of inguinal hernia. Br J Surg 1995;82:274-7. 
[PUBMED] |
| 12. | McCormack K, Scott N, Go PM, Ross SJ, Grant AM. Collaboration the EU Hernia Trialists. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev 2003:CD001785. 
|
| 13. | Bignell M, Partridge G, Mahon D, Rhodes M. Prospective randomized trial of laparoscopic (transabdominal preperitoneal-TAPP) versus open (mesh) repair for bilateral and recurrent inguinal hernia: Incidence of chronic groin pain and impact on quality of life: Results of 10-year follow-up. Hernia 2012;16:635-40. 
[PUBMED] |
| 14. | Morales-Conde S, Socas M, fingerhut A. Endoscopic surgeons' preferences for inguinal hernia repair: TEP, TAPP, or OPEN. Surg Endosc 2012;26:2639-43. 
[PUBMED] |
| 15. | Dan D, Naraynsingh V, Cawich SO, Jonnagoladda R. The history of laparoscopic general surgery in the Caribbean. West Indian Med J 2012;61:465-9. 
|
| 16. | Cawich SO, Cherian CJ, Wilson C, Baker A, Lloyd C, Thomas C. Challenges against the advancement of minimally invasive surgery in Jamaica: A national hospital survey. West Indian Med J 2012;61(Suppl 4):54. 
|
| 17. | Plummer JM, Roberts PO, Leake PA, Mitchell DI. Surgical care in Jamaica in the laparoendoscopic era: Challenges and future prospects for developing nations. Perm J 2011;15:57-61. 
[PUBMED] |
| 18. | Ridings P, Evans DS. The transabdominal pre-peritoneal (TAPP) inguinal hernia repair: A trip along the learning curve. J R Coll Surg Edinb 2000;45:29-32. 
[PUBMED] |
| 19. | Tatulli F, Chetta G, Caputi A, Mastrototaro P, Ruggieri T. Laparoscopic inguinal hernia repair: Audit of our experience with laparoscopic trans-abdominal pro-peritoneal repair (TAPP). Chir Ital 2009;61:47-53. 
[PUBMED] |
| 20. | Anadol AZ, Ersoy E, Taneri F, Tekin E. Outcome and cost comparison of laparoscopic transabdominal preperitoneal hernia repair versus open Lichtenstein technique. J Laparoendosc Adv Surg Tech A 2004;14:159-63. 
|
| 21. | Tzovaras G, Symeonidis D, Koukoulis G, Baloviannis I, Georgopoulou S, Pratsas C, et al. Long-term results after laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair under spinal anesthesia. Hernia 2012;16:973-9. 
|
| 22. | Halverson K, McVay CB. Inguinal and femoral hernioplasty: A 22-year study of the author's method. Arch Surg 1970;101;127-35. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
[Table 1]
|