|


 |
| SURGICAL TECHNIQUE |
|
| Year : 2013 | Volume
: 5
| Issue : 1 | Page : 18-20 |
|
|
A simple technique for adjustment of the femoral offset at the site of hip spacer implantation
Konstantinos Anagnostakos, Olaf Lorbach, Patrick Orth, Katrin Koch
Department of Orthopaedic Surgery, Saarland University Medical Center, Homburg/Saar, Germany
| Date of Web Publication | 21-Sep-2013 |
Correspondence Address:
Konstantinos Anagnostakos
Department of Orthopaedic Surgery, Saarland University Medical Center, Kirrbergerstr. 1, D 66421, Homburg/Saar
Germany
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.118605

 Abstract Abstract | | |
The decrease of femoral offset might play a role in the emergence of hip spacer dislocations, but it has not been discussed in the literature yet. The present work describes a technique for femoral offset adjustment. Either a bended blade plate or a dynamic hip screw can be used. The depth of the insertion and the angle of the particular implant are defined by the size of the offset adjustment required in each case. The described technique is feasible to produce a customized hip spacer, allowing for the preservation of an adequate muscle tension by individual adjustment of the femoral offset between stages. Keywords: Antibiotic-loaded bone cement, femoral offset, hip joint infection, hip spacer, spacer dislocation
How to cite this article:
Anagnostakos K, Lorbach O, Orth P, Koch K. A simple technique for adjustment of the femoral offset at the site of hip spacer implantation. J Surg Tech Case Report 2013;5:18-20 |
How to cite this URL:
Anagnostakos K, Lorbach O, Orth P, Koch K. A simple technique for adjustment of the femoral offset at the site of hip spacer implantation. J Surg Tech Case Report [serial online] 2013 [cited 2016 May 25];5:18-20. Available from: http://www.jstcr.org/text.asp?2013/5/1/18/118605 |
 Introduction Introduction | |  |
Antibiotic-loaded hip spacers are an established method in the treatment of infected total hip arthroplasty (THA), with reported infection eradication rates of >90%. [1] Postoperatively, several mechanical complications might occur such as spacer fractures or dislocations and femoral fractures. Several factors play a role in the emergence of spacer dislocations such as the spacer's geometry and its cervicodiaphyseal angle, the method of production (manually shaped vs. standardized produced), the patient's incompliance, inability of partial weight bearing on the operated extremity, insufficient fixation of the spacer onto the proximal femur, a small spacer head size, large osseous defects of the acetabulum inhibiting a normal spacer articulation, and muscular insufficiency. [2]
Another parameter that might be responsible for spacer dislocation is decreased femoral offset of the implant. To the best of our knowledge, this parameter has not been discussed in the literature yet. Here, we have presented a simple technique for the adjustment of the femoral offset at the site of a hip spacer implantation, which can be applied for both periprosthetic as well as native hip joint infections.
 Surgical Technique Surgical Technique | |  |
The surgical approach can be selected according to pre-existing approaches or the surgeon's preferences. After removal of all prosthetic components (and bone cement in case of cemented implants) as well as debridement of all infected, necrotic, and ischemic tissue parts, the spacer can be manufactured as follows.
For adjustment of the femoral offset, two possible implants are available: Either a dynamic hip screw (DHS) or a blade plate whose cervicodiaphyseal angle has to be adjusted according to the required offset [Figure 1] and [Figure 2]. Both implants have the advantage of various implant sizes so that the femoral offset can be individually adjusted. For small femoras, the use of blade plate is recommended because the DHS is too voluminous for these cases.
Here, the technique is presented with a blade plate. The spacer mold is cut with a scissor through the neck area. First, the antibiotic-loaded cement is inserted into the spacer head mold part. The preformed blade plate is then inserted into the spacer head mold [Figure 3]. The depth of the insertion and the angle of the particular implant are defined by the size of the offset adjustment required in each case. Afterwards, the spacer stem mold is filled with antibiotic-loaded cement and the two parts are assembled [Figure 4]. The plate should be centrally placed into the mold and be completely covered with antibiotic-loaded bone cement. Otherwise, any exposed metal surfaces might pose a possible colonization area for bacteria, which might have survived, and, hence, lead to an infection persistence.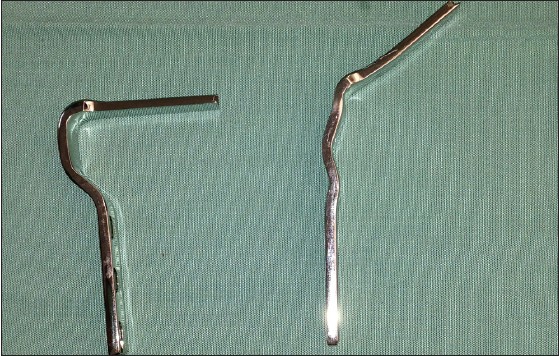 | Figure 1: The technique is presented by the use of a blade plate for femoral offset adjustment. The plate is bent from 90° to approximately 130°
Click here to view |
 | Figure 2: The blade plate is recommended for small femoras and DHS for large femoras
Click here to view |
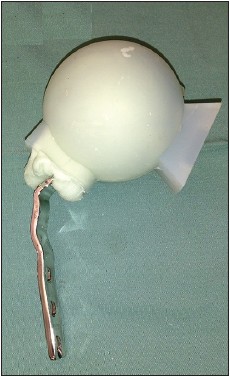 | Figure 3: The technique is demonstrated with a Biomet® silicon mold. The mold is cut with scissors through the spacer neck area. Antibiotic‑loaded bone cement is first inserted into the head mold and
then the bended plate is inserted. The depth of the insertion is defined in accordance with the offset adjustment required in a particular case
Click here to view |
 | Figure 4: The stem mold is filled with antibiotic‑loaded bone cement, and the two parts of the mold are attached to each other with a small gap in between
Click here to view |
Since the decrease of the femoral offset needs to be adjusted, the two mold parts should not be completely attached to each other. The gap between the two mold parts is manually filled with antibiotic-loaded bone cement [Figure 5]. We recommend that this cement ring should be broader than the spacer stem in order to act (1) as a bearing base onto the proximal femur, which might prevent a possible sintering of the spacer into the femur, and (2) contribute to the preservation of an adequate muscle tension. | Figure 5: The gap between the mold parts is manually filled with antibiotic‑loaded bone. This cement ring should be broader than the spacer stem in order to act (1) as a bearing base onto the proximal
femur, which might prevent possible sintering of the spacer into the femur and (2) contribute to the preservation of an adequate muscle tension
Click here to view |
After approximately 10 min, the cement had hardened. The spacer was then removed easily from the mold and inserted into the femur [Figure 6]. X-rays of the hip joint demonstrate the requested increase of the femoral offset as compared with a standard spacer implantation [Figure 7].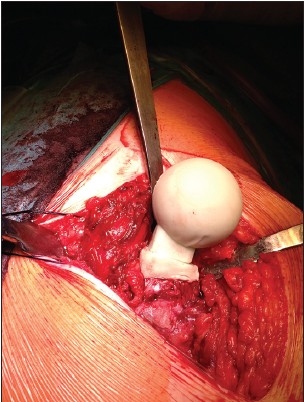 | Figure 6: After hardening of the cement, the spacer is removed from the mold and inserted into the femur
Click here to view |
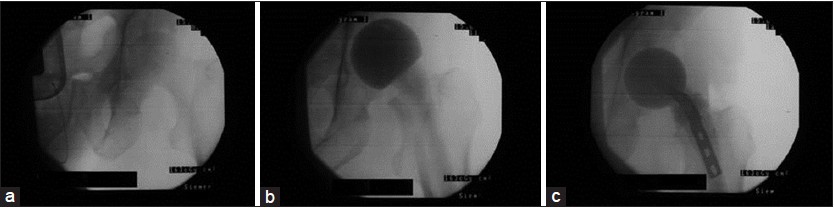 | Figure 7: Intraoperative X‑rays demonstrating the adjustment of the femoral offset in a case of acetabulum osteomyelitis with subsequent septic hip joint arthritis. (a) The natural joint at the beginning of the surgery. (b) If a normal spacer is implanted, a decrease of the femoral offset is evident (notice the distance between the calcar and the os ischium). (c) By implanting a spacer according to the present technique, the femoral offset is increased
Click here to view |
 Discussion Discussion | |  |
The femoral offset is a parameter that might potentially play an important role in the emergence of hip spacer dislocations, but this has not been discussed in the literature. In our department, we have been implanting hip spacers since the late 90's and have observed that hip spacer dislocations are frequent when the femoral offset is decreased as compared with the preoperative configuration, although other predisposing parameters do not exist. A decrease of the femoral offset leads to decreased muscle tension, which might cause spacer dislocations, despite an intact bone and muscle situation and a normal spacer articulation. This accounts for periprosthetic joint infections with a high-offset stem as well as septic arthritis cases with a large femoral neck.
To the best of our knowledge, only one study evaluated hip spacer dislocations with regard to the hip joint biomechanics. Leunig et al., recognized that the geometrical form of the spacer plays an important role. [3] In spacers that were free of complications, the neck-to-head ratio was significantly lower (0.76 ± 0.05) than in those with dislocations (0.96 ± 0.19). A second factor associated with failure was an insufficient deep anchorage in the intramedullary canal (22 ± 33 mm in the failure group), while complication-free spacers were on average attached to a depth of 57 ± 41 mm.
Commercially available and custom-made hip spacers have, in the great majority of the cases, a decreased femoral offset in comparison with the offset of prosthesis stems or the natural offset in case of septic arthritis. The present technique describes a method that can be easily and quickly applied during surgery. The use of a bended blade plate in small femoras and/or a DHS in large femoras allows individual adjustment of the femoral offset, and hence preserves a normal muscle tension. The insertion of a DHS into a spacer has been described as an endoskeleton for the enhancement of the mechanical stability, [4] but not as an offset adjustment. This technique can be used with commercially available silicon molds such as the Biomet® mold and also with custom-made molds. In our experience, the individual adjustment of the femoral offset and the thereby preserved muscle tension are also beneficial for the later prosthesis (re)implantation. The joint biomechanics are preserved to an almost normal condition between stages, thus providing an excellent precondition for the preoperative planning of the prosthesis (re)implantation.
 References References | |  |
| 1. | Anagnostakos K, Fürst O, Kelm J. Antibiotic-impregnated PMMA hip spacers: Current status. Acta Orthop 2006;77:628-37. 
|
| 2. | Anagnostakos K, Jung J, Schmid NV, Schmitt E, Kelm J. Mechanical complications and reconstruction strategies at the site of hip spacer implantation. Int J Med Sci 2009;6:274-9. 
[PUBMED] |
| 3. | Leunig M, Chosa E, Speck M, Ganz R. A cement spacer for two-stage revision of infected implants of the hip joint. Int Orthop 1998;22:209-14. 
[PUBMED] |
| 4. | Peng KT, Kuo LT, Hsu WH, Huang TW, Tsai YH. The effect of endoskeleton on antibiotic impregnated cement spacer for treating deep hip infection. BMC Musculoskelet Disord 2011;12:10. 
[PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7]
|