|


 |
| CASE REPORT |
|
| Year : 2013 | Volume
: 5
| Issue : 1 | Page : 41-44 |
|
|
Single incision laparoscopic surgery for a large endometriotic cyst
Ying Woo Ng1, Catherina Josephine Goenadi2, Yoke Fai Fong2
1 Department of Obstetrics and Gynaecology, National University Hospital, Singapore
2 Yong Loo Lin School of Medicine, National University of Singapore, Singapore
| Date of Web Publication | 21-Sep-2013 |
Correspondence Address:
Ying Woo Ng
Department of Obstetrics and Gynaecology, National University Hospital, 1E Lower Kent Ridge Road, NUHS Tower Block, Level 12, 119228
Singapore
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.118628

 Abstract Abstract | | |
We describe a technique for the treatment of large benign ovarian cysts by single port laparoscopic surgery via the umbilical approach. X-cone single port system (Karl Storz) was employed in this surgery. Prebent atraumatic grasping forceps were used in conjunction with the straight laparoscopic instruments. We propose using a "to-fro" peeling technique in the z-axis in SPLS cystectomy. Combined use of prebent and straight laparoscopic instruments enables the cystectomy to be performed in the z-axis, thereby avoiding instruments crossing and hands collision outside the abdomen. The proposed technique proved to be feasible, easy to employ, and safe in SPLS cystectomy, with the additional benefi t of superior cosmetic outcome. Keywords: Cystectomy, laparoscopy, ovarian, single incision, single incision laparoscopic surgery, single port
How to cite this article:
Ng YW, Goenadi CJ, Fong YF. Single incision laparoscopic surgery for a large endometriotic cyst. J Surg Tech Case Report 2013;5:41-4 |
How to cite this URL:
Ng YW, Goenadi CJ, Fong YF. Single incision laparoscopic surgery for a large endometriotic cyst. J Surg Tech Case Report [serial online] 2013 [cited 2016 May 25];5:41-4. Available from: http://www.jstcr.org/text.asp?2013/5/1/41/118628 |
 Introduction Introduction | |  |
In the last decade, laparoscopy has become the standard treatment for many gynecological conditions. [1],[2] Today, laparoscopy is hailed as the standard approach in the surgical treatment of benign adnexal pathology. [1],[2] Attempts to minimize access-related injuries and complications resulted in development of single port laparoscopic surgery (SPLS), which, because of the decreased number of ports used, may be the next generation of minimally invasive surgery. The advantages of single-port surgery have been reported to include reduced perioperative morbidity, a quicker recovery time because of less postoperative pain, less blood loss, fewer complications, and certainly superior cosmetic results. [3],[4],[5]
A number of reports have reported on the success of performing adnexectomy using SPLS. [6],[7],[8],[9] Yet few reports have published on the SPLS approach in treating large ovarian cysts. [10],[11],[12] The restricted intraabdominal working space in large ovarian cysts poses a technical challenge. Moreover, difficult convergence of operating instruments and competition for operating space outside the abdomen during the SPLS makes the procedure demanding, especially when one uses conventional instruments.
Herein, we describe a minimally invasive technique for SPLS for the treatment of a 10 cm ovarian cyst, which reduces the technical difficulties involved in such surgery.
 Case Report Case Report | |  |
A 27-year-old single nulliparous lady (body mass index = 17.5) presented with a 3-day history of left iliac fossa and suprapubic pain which progressively got worse despite analgesia. The pain score of 8/10 upon presentation. There was no vaginal bleeding or discharge. She reported dysmenorrheal during her periods, requiring analgesia.
Abdominal examination revealed a normal-sized uterus with tenderness over the left iliac fossa and suprapubic region with no signs of peritonism. Abdominal ultrasonography revealed a left ovarian cyst measuring approximately 8 × 5 cm (suggestive of endometrioma) without septae or echogenicity or any surface excrescences. Color Doppler examination of the cyst revealed no abnormal vasculature. The right ovary and uterus was normal in appearance and there was no ascites. Preoperative CA-125 levels were elevated at 73.7 U/mL but other ovarian tumor markers were within normal limit. The patient was counseled for diagnostic laparoscopy with subsequent ovarian cystectomy.
 Operative Procedures Operative Procedures | |  |
The laparoscopic procedure was performed under general anesthesia. Patient was positioned in the lithotomy with Lloyd-Davies position and was cleaned, draped, and catheterised. A curette was inserted vaginally as uterine manipulator.
The surgical instruments used during the surgery were X-cone single port system [Figure 1], a rigid 30°, 5-mm diameter, 45-cm long laparoscope in combination with, a rigid prebent atraumatic grasping forceps, a straight Reddick grasping forceps [Figure 2] and a standard straight Robi Kelly bipolar. X-cone single port system is a reusable, low-cost single site trocar with four integrated access ports (X-Cone; Karl Storz, Tuttlingen, Germany).
A 1.5 cm vertical incision was made at the umbilicus. Pneumoperitoneum was created using open Hasson's entry techniques. Diagnostic laparoscopy was performed prior to the decision for SPLS. Laparoscopy revealed a normal-sized uterus with right ovarian endometriotic cyst measuring approximately 10 cm in diameter [Figure 3] with filmy adhesions between the cyst and ovarian fossa. Other pelvic organs were normal. As there were only minimal adhesions around the ovarian cyst, a decision was made to proceed with SPLS. | Figure 1: X-cone is reusable, low-cost single site trocar with multiple ports
Click here to view |
X-cone single port system was then inserted. A 5-mm 45 cm 30° laparoscope was passed through the port for visualization. A straight Reddick grasper and a prebent 5-mm atraumatic grasper were inserted into the remaining two ports [Figure 4]. | Figure 4: Combined use of prebent and straight forceps through X-cone single port system
Click here to view |
Vertical incision was made over the cyst and the incision was widened using laparoscopic scissor. The overlying ovarian tissue was teased away and the plane between the cyst and ovarian tissue dissected using Reddick straight forceps. Cyst was punctured under direct vision and its content was aspirated with a suction-irrigation device with minimal spillage as the incision edge was held up by the prebent atraumatic grasping forceps. Cyst wall was then peeled off from the ovarian tissue using both the prebent and straight forceps in a "to-fro" manner along the z-axis: The prebent forcep pushed the top part of the cyst wall distally and the straight forcep pulled the inferior part proximally thus providing traction and counter-traction to facilitate stripping of the cyst. The cyst wall was then removed via the umbilical incision. Hemastasis was secured using bipolar forceps. Copious peritoneal lavage was carefully performed until clear return. Surgicel was then placed over the inner surface of the right ovary. The sheath was closed with 2-0 Vicryl. Last, the skin was repaired with Monocryl.
 Results Results | |  |
X-cone port placement was successful in creating pneumoperitoneum with no-minimal air leak. No vascular or visceral injuries or intraoperative port site bleeding occurred. Operative time was 125 min and there was minimal blood loss. After surgery, there was no wound hematoma, wound infection, or delayed bleeding. Patient was discharged well with optional analgesia. Final pathological analysis confirmed endometriotic cyst. Patients conveyed high satisfaction toward cosmetic result and postoperative pain control with a satisfaction score of 9 on a scale of 1-10 upon follow-up 2 months later [Figure 5].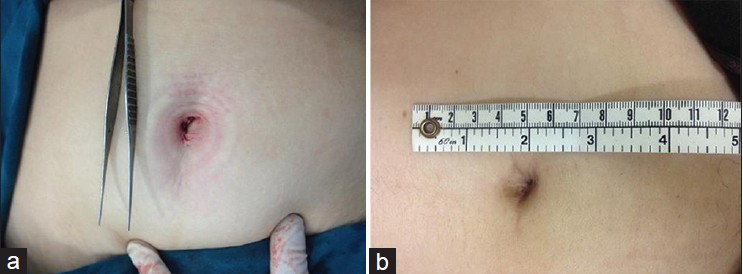 | Figure 5: (a) Umbilical scar immediately after the surgery and (b) 8-week after the surgery
Click here to view |
 Discussion Discussion | |  |
Benign ovarian tumors account for 90% of all ovarian tumors. Benign lesions are usually unilateral, cystic, mobile and smooth, without ascites, and are frequently found in younger age groups. [13] Although, we noticed that in this patient, there is an elevated Ca-125, we feel that it is related to the endometriosis pathology.
We used X-cone system (Karl Storz), a new single port trocar device that allows simultaneous passage of various laparoscopic instruments through one small opening and also has the advantage of being reusable thereby reducing overall surgical cost. We advocate the use of a 5-mm, 30° long 45-cm telescope which helped to achieve both adequate visualization and to avoid a clashing of the operating instruments and the optic outside the abdomen. The use of rigid prebent instruments is crucial to widen the surgeon's movements outside of the abdominal cavity, avoiding crossing between the instruments and the camera, and to allow lateral movements inside the abdomen.
The highlight of our technique was the combined use of prebent instrument and standard straight instrument to provide traction-countertraction during cyst wall peeling in a "to-fro" manner along the z-axis which is parallel to the instrument axis unlike the standard laparoscopic traction. The advantage of this technique is that since both instruments are working together parallel to each other in the z-axis, crossing and collision between instruments outside the abdomen could be minimized.
Concerning the postoperative outcome, our patient was very happy with the cosmetic of her scar rating her satisfaction level at 9 out of 10 in a 1-10 scale. In addition, a single minimal incision of the peritoneum could suggest a shorter recovery, as observed in our patient. Furthermore, no further complications have been observed in our patient.
 Conclusion Conclusion | |  |
SPLS is an innovative approach that is rapidly gaining recognition around the world. In this study, using the described technique, we support the use of SPLS in laparoscopic cystectomy for ovarian cysts up to 10 cm. SPLS proved to be feasible and safe in this case with superior cosmetic result.
 References References | |  |
| 1. | Mettler L, Jacobs V, Brandenburg K, Jonat W, Semm K. Laparoscopic management of 641 adnexal tumors in Kiel, Germany. J Am Assoc Gynecol Laparosc 2001;8:74-82. 
[PUBMED] |
| 2. | Medeiros LR, Fachel JM, Garry R, Stein AT, Furness S. Laparoscopy versus laparotomy for benign ovarian tumours. Cochrane Database Syst Rev 2005;3:CD004751. 
[PUBMED] |
| 3. | Romanelli JR, Earle DB. Single-port laparoscopic surgery: An overview. Surg Endosc 2009;23:1419-27. 
[PUBMED] |
| 4. | Fader AN, Escobar PF. Laparoendoscopic single-site surgery (LESS) in gynecologic oncology: Technique and initial report. Gynecol Oncol 2009;114:157-61. 
[PUBMED] |
| 5. | Pfluke JM, Parker M, Stauffer JA, Paetau AA, Bowers SP, Asbun HJ, et al. Laparoscopic surgery performed through a single incision: A systematic review of the current literature. J Am Coll Surg 2011;212:113-8. 
[PUBMED] |
| 6. | Fagotti A, Fanfani F, Rossitto C, Marocco F, Gallotta V, Romano F, et al. Laparoendoscopic single-site surgery for the treatment of benign adnexal disease: A prospective trial. Diagn Ther Endosc 2010;2010:108258. 
|
| 7. | Fagotti A, Fanfani F, Marocco F, Rossito C, Gallotta V, Scambia G. Laparoendoscopic single-site surgery (LESS) for ovarian cyst enucleation: Report of first 3 cases. Fertil Steril 2009;92:1168.e13-6. 
|
| 8. | Mereu L, Angioni S, Melis GB, Mencaglia L. Single access laparoscopy for adnexal pathologies using a novel reusable port and curved instruments. Int J Gynecol Obstet 2010;109:78-80. 
|
| 9. | Capar M, Balci O, Acar A, Colakoglu MC. Management of ovarian cysts by laparoscopic extracorporeal approach using single ancillary trocar. Taiwan J Obstet Gynecol 2009;48:380-4. 
[PUBMED] |
| 10. | Lee LC, Sheu BC, Chou LY, Huang SC, Chang DY, Chang WC. An easy new approach to the laparoscopic treatment of large adnexal cysts. Minim Invasive Ther Allied Technol 2011;20:150-4. 
[PUBMED] |
| 11. | Garg P, Misra S, Thakur JD, Song J. Single incision laparoscopic surgery ovarian cystectomy in large benign ovarian cysts using conventional instruments. J Minim Access Surg 2011;7:232-5. 
[PUBMED] |
| 12. | Yi SW. Minimally invasive management of huge ovarian cysts by laparoscopic extracorporeal approach. Minim Invasive Ther Allied Technol 2012;21:429-34. 
[PUBMED] |
| 13. | Sanfilippo JS, Rock JA. Surgery for benign diseases of the ovary. In: Rock JA, Jones HW 3 rd , editors. Te Linde's Operative Gynecology. 9 th ed. Philadelphia: Lippincott Williams and Wilkins; 2003. p. 639-59. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
|