|


 |
| CASE REPORT |
|
| Year : 2014 | Volume
: 6
| Issue : 2 | Page : 49-54 |
|
|
A Novel surgical pre-suturing technique for the management of ankyloglossia
Mayur Khairnar1, Babita Pawar2, Darshana Khairnar1
1 Private Practice?, Precision Dental Clinic, Mumbai, Maharashtra, India
2 Department Periodontology, Rural Dental College, Loni, Maharashtra, India
| Date of Web Publication | 18-Dec-2014 |
Correspondence Address:
Mayur Khairnar
Precision Dental Clinic and Implant Centre, Shop No. 13, New Geetanjali CHS Ltd., Near K. T. Vision Multiplex, Anand Nagar, Vasai West, Thane 401 202, Maharashtra
India
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.147259

 Abstract Abstract | | |
Ankyloglossia or "tongue-tie" is a congenital anomaly caused by tight lingual frenulum that abnormally connects the tongue base to the floor of the mouth. Ankyloglossia can results in difficulty during speech and deglutition. This case series presents a novel surgical technique in the management of ankyloglossia in using presuturing technique in which different sets of sutures are given on lingual frenum before severing it. This results in reduced opening of the wound, minimal bleeding, pain and discomfort. Two male patients with severe ankyloglossia had been managed with this technique and after 2 years of follow-up of these cases showed satisfactory protrusive and lateral movement of the tongue with minimal scarring and discomfort. Keywords: Ankyloglossia, lingual frenectomy, tongue tie
How to cite this article:
Khairnar M, Pawar B, Khairnar D. A Novel surgical pre-suturing technique for the management of ankyloglossia. J Surg Tech Case Report 2014;6:49-54 |
How to cite this URL:
Khairnar M, Pawar B, Khairnar D. A Novel surgical pre-suturing technique for the management of ankyloglossia. J Surg Tech Case Report [serial online] 2014 [cited 2016 May 10];6:49-54. Available from: http://www.jstcr.org/text.asp?2014/6/2/49/147259 |
 Introduction Introduction | |  |
Ankyloglossia or "tongue-tie" is a congenital anomaly caused by an abnormally thick tight lingual frenulum (the band of tissue that connects the tongue base to the floor of the mouth) resulting in limitation of tongue movement. Wallace [1] defined Ankyloglossia (tongue tie) as "a condition in which the tip of the tongue cannot be protruded beyond lower incisor teeth because of a short lingual frenulum, often containing scar tissue".
Ankyloglossia is more commonly found in males than females, [2] with incidence of 1.72% to 10.7% - in breast feeding patients. [3] Ankyloglossia leads to inability to extend the tip of tongue beyond the vermillion border of the lips or a line joining the lip commissures, along with speech impairment, midline diastema, oral motor dysfunction and mandibular lingual gingival recession.
The severity of ankyloglossia is variable and ranges from a slight but abnormal attachment of frenum restricting little tongue movement (partial ankyloglossia) to a condition with the tongue fixed to the floor of the mouth completely (complete ankyloglossia).
Kotlow [4] has classified severity ankyloglossia on the basis of Length of the "free tongue" [Table 1] Free tongue is defined as the length of the tongue from the insertion of the lingual frenum into the base of the tongue to the tip of the tongue. [4] A free tongue measurement both in older patients and infants can be measured using Kotlow's classification of ankyloglossia. Usually, patient with ankyloglossia demonstrates symptoms like difficulty in breast feeding (infants), improper pronunciation of certain consonants and diphthongs ('letters such as t, d, r, n and l, in sounds and words such as ta, te, time, water, and cat, etc.), unsatisfactory oral hygiene due to limited cleansing action of tongue and difficulty in achieving social movements of tongue like licking an ice-cream, sucking, playing musical instrument particularly wood wind or kissing, etc.
Several conservative, as well as surgical options, exist for the management of tongue tie. It includes observation, speech therapy, otolaryngotherapy, frenotomy, frenectomy, Z-plasty and laser frenectomy. If intervention of speech and otolaryngotherapist fails to resolve speech and tongue related problems then it may be appropriate to consider surgical protocol. The literature suggests that surgical interventions are absolutely safe at any age including infants, toddlers and adults but strictly requires postsurgical speech therapy to achieve pleasing results.
Surgical procedures indicated for ankyloglossia are highly predictable but shows poor patient compliance, more postoperative pain and swelling. Furthermore, bleeding associated with conventional frenectomy and Z-plasty is of great extent. Frenectomy using laser can overcome this problem, but lasers are not readily available at every operating centre.
The aim of this case series was to present a novel surgical maneuver for management of Kotlow's Class II and IV ankyloglossia, which help reduce the intra-operative bleeding, and postoperative pain, swelling and discomfort. And also evaluated the postoperative free movement of tongue and scarring after 2 years follow-up period.
 CASE REPORTs CASE REPORTs | |  |
Case 1
A 19-year-old male reported with a complaint of restricted tongue movement and difficulty in speech. Clinical examination showed the presence of Kotlow's Class II ankyloglossia [Figure 1].
Case 2
A 21-year-old man reported with a complaint of difficulty in speech and deglutition. History of speech therapy 6 months back with no benefit from it. He also had difficulty in licking, sucking or whistling. The ear, nose, throat and other physical examination was normal. Intra oral examination revealed Kotlow's Class IV ankyloglossia [Figure 2]. Any attempt to protrude the tongue resulted in clefting at the tip of the tongue and retrusion of tongue blanched the tissue lingual to anterior teeth.
Both the patients were neither be able to protrude their tongue beyond the vermillion border of lower and upper lip nor able to utter letter sound "l," "t," "d," "n," "s," and "th" clearly. In both the cases, aetiology of ankyloglossia was unknown, and there was no association with any syndrome. There was no frenum related recession on the lingual aspect of mandibular central incisors. After assessing, an informed consent was attained, and lingual frenectomy was planned.
 Investigations Investigations | |  |
All necessary blood investigation report required before any surgical procedure was evaluated and was found to be within normal limits.
 Treatment Treatment | |  |
Surgical procedure
The patient was advised to rinse the mouth with 10 ml 0.2% chlorhexidine mouthwash before commencement of surgical procedure. Xylocaine with 1:80,000 adrenaline (Lignox Warren Pharma; Navi Mumbai, Maharashtra, India) was used for local infiltration anesthesia. 0.5-1 ml of solution was deposited bilaterally at the base of the tongue, floor of the mouth and toward the geniod tubercle on the lingual aspect of mandible.
A retraction suture (3-0 silk) was placed at the tip of the tongue to facilitate retraction and visibility in the area of the operating field. Following this two different set of sutures were planned. The first set included 2-4 simple interrupted sutures placed in a vertical line extending from the tip of the tongue to the base of the frenum. The next set included 2-3 simple interrupted sutures, location being placed anterior and parallel to the previous line of sutures on the lingual frenum in a vertical line [Figure 3]. In this case, both first and second set of sutures included only two interrupted sutures. Suturing was done cautiously so as to prevent tying of wharton's duct, an opening of the submandibular gland. The frenum was held with hemostat [Figure 4] between two vertical rows of sutures then with No. 15 blade, (Schwanno morton) frenum was severed carefully. Presuturing of frenum before severing prevented excessive opening of diamond shape wound and provided greater hemostatis [Figure 5].
Following this tongue was checked for any muscle tension, if any it was relieved by carrying blunt dissection in floor of the mouth by using haemostat [Figure 5]. Patient was instructed to assess freeness of tongue through protruding and sweeping upper and lower lip and corner of the mouth without much straining. An accessory suture was placed in the floor of the mouth in the area where blunt dissection was carried out [Figure 6].
Patients were prescribed antibiotic amoxicillin 500 mg and analgesics Ketorolac 10 mg 3 times a day for 7 days and 3 days respectively and advised to use 2% chlorhexidine twice daily for 2 weeks. Postoperative instructions included sucking of ice chips during first 24 hours, performance of postoperative tongue exercises after first 24 hours, and avoidance of any hot, hard or spicy food stuff. The postoperatively tongue exercise included touching of tongue to the palatine rugae while keeping mouth opened, rolling tongue side to side touching corner of the mouth, stretching of the tongue with a protrusive action. Patients were instructed to continue this exercise 3-4 times daily for 2 min until the incision healed. Sutures were removed carefully 1-week after surgery.
 Outcome and Follow-Up Outcome and Follow-Up | |  |
Postoperative evaluation
The primary closure of the wound resulted in an uneventful healing with the primary intention after 1-week [Figure 7]. Thereafter, patients were advised to initiate speech therapy.
According to patient's perception, visual analogue scale score for pain during complete surgical procedure, and subsequent week was recorded to be 4 and 2 for case1 and case 2 respectively. There was no postoperative complication associated with the procedure like infection, bruising on floor of the mouth, submandibular gland swelling, lingual par aesthesia, numbness tongue tip during next week of surgery.
Postoperative 2 years follow-up of both the cases revealed minimal scaring, satisfactory protrusive and lateral movement of the tongue without any discomfort [Case 2: [Figure 8], [Figure 9], [Figure 10] and Case 1: [Figure 11]. Patients also overcame the difficulty during speech and active social movement of the tongue like act of licking, sucking, whistling, etc.
 Discussion Discussion | |  |
Ankyloglossia is a rare congenital oral anomaly that can cause difficulty with breast-feeding, speech delivery. Kotlow [4] had described nine structural guidelines to determine the need for surgical management of lingual frenulum:
- If the tip of the tongue cleft during the act of protrusion
- If the tip of the tongue is not able to sweep the upper and lower lips easily, without straining
- If retrusion of tongue, blanches the tissue lingual to anterior teeth
- If tongue places excessive forces on mandibular anterior teeth
- If the frenum interferes with normal deglutition process
- If lingual frenum creates diastema between mandibular central incisors
- If child experiences speech difficulty due to limited tongue movements
- If infants, shows abrasion at underside of the tongue, and
- If the frenum prevents infant from attaching to mother's nipple during nursing.
The prevalence is higher in neonates [3] (1.72-10.7%) than in children, adolescents, or adults (0.1-2.08%). [5]
Ankyloglossia is also found to be associated with some rare syndromes such as X-linked cleft palate syndrome, [6] Kindler syndrome, [7] van der Woude syndrome, [8] and Opitz syndrome. [9] Nevertheless, most ankyloglosia are observed in individuals without any other congenital anomalies or diseases.
Ankyloglossia is always associated with foreshortening of the genioglossus muscle, just mere frenotomy/snipping of the lingual frenum may not allow free and coordinated movement of the tongue. If done in such cases, postoperative recurrence of frenum reattachment is very high. Although, such problem of frenulum reattachment can be overcome by conventional frenectomy or Z-plasty (frenuloplasty) procedures but it results in to opening of extensive diamond shape wound in case of frenectomy [10] and zig-zag wound in case of Z-plasty/4 flap Z-plasty. [11] Greater the opening of wound greater is the bleeding, more difficult is to achieve the hemostatis and hence wound approximation. Also, manual dexterity to manage such situiation is required to be excellent. There is also no sufficient evidence in the literature favouring any one of above surgical treatment options for management of ankyloglossia. Though laser frenectomy [12],[13] shows pleasing results with blood-less approach, but it doubts to relieve muscle attachment. Hence, chances of recurrences cannot be neglected. Long term follow-up studies are required to confirm its result. Also, Lasers are not readily available at every clinical set-up. However, in contrast to conventional frenectomy and Z-plasty, presuturing technique provides excellent hemostatis, no opening of greater wound and appropriate primary wound closure. In the present case series, this presuturing technique offered minimal postoperative pain and morbidity, no swelling, immediate tongue freeness with minimal or no tension on lingual frenum and minimal scarring and no reattachment of lingual frenum after 2 years of follow-up [Figure 8], [Figure 9] [Figure 10], [ Figure 11].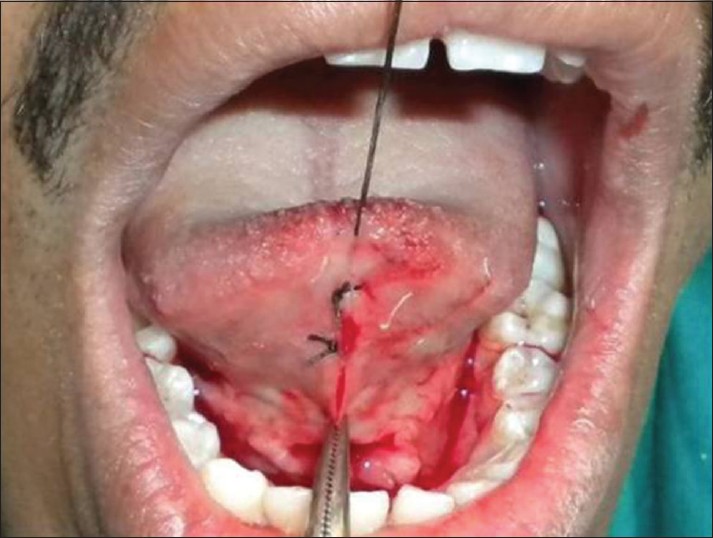 | Figure 5: Presuturing prevents excessive opening of diamond shape wound (Case 2)
Click here to view |
 | Figure 10: Tongue position on left and right lateral movement after 2 years (Case 2)
Click here to view |
Improvement in speech, deglutition, and other social movement of the tongue were also excellent 2 years after surgery. Improved tongue movement and function was not only attributed to the surgical procedure carried out but also to postsurgical tongue exercises given to the patient.
Postoperative exercises following tongue-tie surgery were not intended to increase muscle-strength, but to: 14
- Develop new muscle movements, particularly those involving tongue-tip elevation and protrusion, inside and outside of the mouth
- Increase kinaesthetic awareness of the full range of movements the tongue and lips can perform
- Encourage tongue movements related to cleaning the oral cavity, including sweeping the insides of the cheeks, fronts and backs of the teeth, and licking right around both lips.
Thus, this technique provides promising result in management of severe ankyloglossia with just suturing prior to lingual frenectomy. However, to confirm the potential of this surgical technique long term interventional randomized clinical trial need to be carried out.
 Learning Points/Take Home Messages Learning Points/Take Home Messages | |  |
- This surgical approach suggests suturing of lingual frenum prior to severing of frenum.
- Presuturing approach avoids excessive bleeding and postoperative discomfort by preventing opening of large wound after lingual frenectomy.
- One must be very careful not to suture opening of sublingual or any other salivary gland in the floor of the mouth. This can avoid any salivary retention cyst or mucocele.
- One must not forget to relieve muscle tension by blunt dissection so as to avoid recurrence and reattachment.
- The postoperative tongue exercise during healing plays crucial role in achieving tongue freeness.
 References References | |  |
| 1. | Wallace AF. Tongue tie. Lancet 1963;2:377-8.  [ PUBMED] |
| 2. | Nevile B, Damm D, Allen C, Bouquot J. Developmental defects of the oral and maxillofacial region. Oral and Maxillofacial Pathology. 2 nd ed. Philadelphia: Saunders; 2002. p. 1-48.  |
| 3. | Ballard JL, Auer CE, Khoury JC. Ankyloglossia: Assessment, incidence, and effect of frenuloplasty on the breastfeeding dyad. Pediatrics 2002;110:1-6.  |
| 4. | Kotlow LA. Ankyloglossia (tongue-tie): A diagnostic and treatment quandary. Quintessence Int 1999;30:259-62.  |
| 5. | Moore GE, Ivens A, Chambers J, Farrall M, Williamson R, Page D C, et al. Linkage of an X-chromosome cleft palate gene. Nature 1987;326:91-2.  [ PUBMED] |
| 6. | Hacham-Zadeh S, Garfunkel AA. Kindler syndrome in two related Kurdish families. Am J Med Genet 1985;20:43-8.  [ PUBMED] |
| 7. | Burdick AB, Ma LA, Dai ZH, Gao NN. van der Woude syndrome in two families in China. J Craniofac Genet Dev Biol 1987;7:413-8.  |
| 8. | Brooks JK, Leonard CO, Coccaro PJ Jr. Opitz (BBB/G) syndrome: Oral manifestations. Am J Med Genet 1992;43:595-601.  |
| 9. | Chaubal TV, Dixit MB. Ankyloglossia and its management. J Indian Soc Periodontol 2011;15:270-2.  [ PUBMED]  |
| 10. | Heller J, Gabbay J, O'Hara C, Heller M, Bradley JP. Improved ankyloglossia correction with four-flap Z-frenuloplasty. Ann Plast Surg 2005;54:623-8.  |
| 11. | Haytac MC, Ozcelik O. Evaluation of patient perceptions after frenectomy operations: A comparison of carbon dioxide laser and scalpel techniques. J Periodontol 2006;77:1815-9.  |
| 12. | Doshi Y, Shah M, Khandge N, Sanghavi A. Advantages of diode laser (940 Nm) over surgical blade in management of ankyloglossia: A case report. J Oral Laser Appl 2010;10:165-9.  |
| 13. | Darshan HE, Pavithra PM. Tongue tie: From confusion to clarity: A review. Int J Dent Clin 2011;3:48-51.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10], [Figure 11]
[Table 1]
|