|


 |
| CASE REPORT |
|
| Year : 2015 | Volume
: 7
| Issue : 1 | Page : 17-19 |
|
|
Malignant transformation of vagal nerve schwannoma in to angiosarcoma: A rare event
Sangeet Kumar Agarwal1, Manish Munjal1, Devinder Rai1, Seema Rao2
1 Department of Otolaryngology and Head, Neck Surgery, Ganga Ram Institute of Post Graduate and Medical Research, Sir Ganga Ram Hospital, New Delhi, India
2 Department of Pathology, Division of Histopathology, Ganga Ram Institute of Post Graduate and Medical Research, Sir Ganga Ram Hospital, New Delhi, India
| Date of Web Publication | 29-Jun-2016 |
Correspondence Address:
Sangeet Kumar Agarwal
Department of Otolaryngology and Head, Neck Surgery, Ganga Ram Institute of Post Graduate and Medical Research, Sir Ganga Ram Hospital, New Delhi
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2006-8808.184941

 Abstract Abstract | | |
Schwannomas are benign, rare peripheral nerve sheath tumors that occur in the head and neck region. Some physicians opt to closely observe cases of schwannoma of the neck on an outpatient basis rather than to perform radical surgery. However, there is a possibility, albeit rare, of malignant transformation of a benign schwannoma. Here, we are reporting the first case from the Indian subcontinent which was transformed into the angiosarcoma from benign vagal schwannoma over a long period. A 47-year-old male patient complaining of left sided neck swelling since last 12 years, swelling was insidious in onset, gradually progressive very slowly. In last 2 months, the size of the swelling was suddenly increased. On examination, there was an approximately 6 cm × 6 cm of size, firm, nodular, well-defined, nontender swelling in the left lateral part of the neck. Fine-needle aspiration cytology (FNAC) revealed paraganglioma and magnetic resonance imaging demonstrated very clearly a tumor, its morphology, and its relation to the surrounding structures, the tumor was thought to be a vagal schwannoma. Surgery was done, and the whole of the tumor was removed in toto. On final histopathological diagnosis, the tumor was proved to be angiosarcoma developed from vagal schwannoma. Postoperative chemotherapy was given but due to distant metastasis, the patient died. Long standing neck masses can convert into malignancy as in our case, therefore, work up of the patient should be done properly. Multiple FNAC should be done because single FNAC can give the false negative result as in our case. This was our diagnostic drawback not to do multiple computed tomography guided FNAC. Keywords: Angiosarcoma, malignant transformation, vagal schwannoma
How to cite this article:
Agarwal SK, Munjal M, Rai D, Rao S. Malignant transformation of vagal nerve schwannoma in to angiosarcoma: A rare event. J Surg Tech Case Report 2015;7:17-9 |
How to cite this URL:
Agarwal SK, Munjal M, Rai D, Rao S. Malignant transformation of vagal nerve schwannoma in to angiosarcoma: A rare event. J Surg Tech Case Report [serial online] 2015 [cited 2018 Jul 1];7:17-9. Available from: http://www.jstcr.org/text.asp?2015/7/1/17/184941 |
 Introduction Introduction | |  |
Vagal schwannomas are benign, rare peripheral nerve sheath tumors in the head and neck region. Some physicians opt to closely observe cases of schwannoma of the neck on an outpatient basis rather than to perform radical surgery. However, there is a possibility, albeit rare, of malignant transformation of a benign schwannoma.[1],[2] Here, we are reporting the first case from the Indian subcontinent, which was transformed into the angiosarcoma from benign vagal schwannoma over a long period.
 Case Report Case Report | |  |
A 47-year-old male patient presented with a left sided neck swelling since last 12 years, insidious in onset, and slowly progressive. In last 2 months, the swelling has suddenly increased in size.
On examination, there was a firm, nodular, well-defined, nontender swelling of approximately 6 cm × 6 cm size, in the left lateral part of the neck. Fine-needle aspiration (FNA) cytology revealed paraganglioma and magnetic resonance
imaging (MRI) demonstrated a tumor thought to be a vagal schwannoma with its morphology, and its relation to the surrounding structures [Figure 1].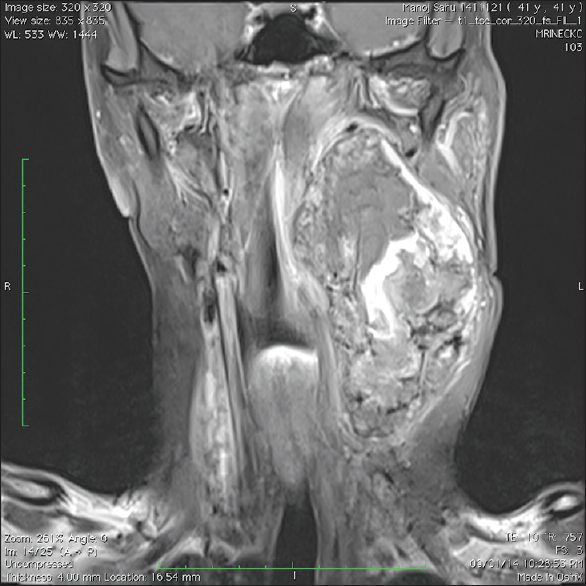 | Figure 1: Contrast-enhanced magnetic resonance imaging, T1-weighted fat saturated coronal image shows a large isointense signal intensity mass admixed with hyperintense signal intensity
Click here to view |
During surgery, the tumor was found to be arising from the vagus nerve and adherent to the common carotid artery through the artery was unaffected by the tumor. The tumor was dissected from all its attachments up to pterygoid plates. Complete tumor resection was achieved by removing the involved segment of the vagus nerve. The postoperative course was uneventful.
Pathologic findings showed a solid gray-white tumor with large areas of hemorrhage, necrosis, and cystic changes. The tumor measured 11 cm × 6.5 cm × 3.5 cm.
Microscopic examination showed verocay bodies (Antoni A region), focal admixed hypocellular areas with edematous vascular stroma and haphazardly arranged tumor cells (Antoni B region). Multiple areas revealed a vasoformative tumor composed of numerous, irregular, anastomosing vascular spaces with dissecting pattern and with high mitotic activity, and the presence of atypical mitosis. The vascular channels were lined by pleomorphic, endothelial cells showing large ovoid nuclei, heterogenous chromatin, and prominent nucleoli [Figure 2].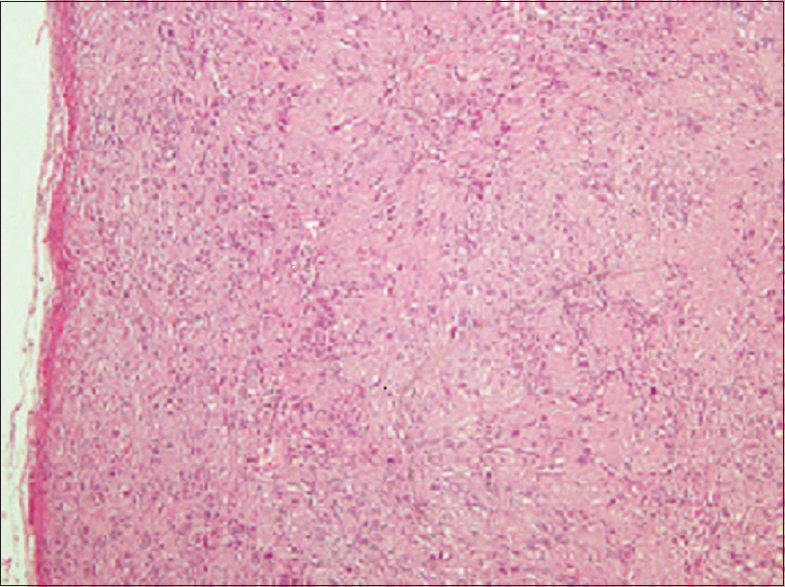 | Figure 2: Section showing a well-encapsulated benign spindle cell tumor with characteristic Verocay bodies, consistent with schwannoma (H and E, ×5)
Click here to view |
On immunohistochemistry-spindle cell tumor (nerve sheath tumor) component was positive with S-100 and negative for CD31. Vasoformative tumor areas were positive for CD31 and negative for CD34 and S-100. Ki-67 showed the high proliferation index in vasoformative tumor areas (40–50%) and was only about 1% in nerve sheath tumor areas. The final histopathological diagnosis was angiosarcoma arising in a benign schwannoma [Figure 3].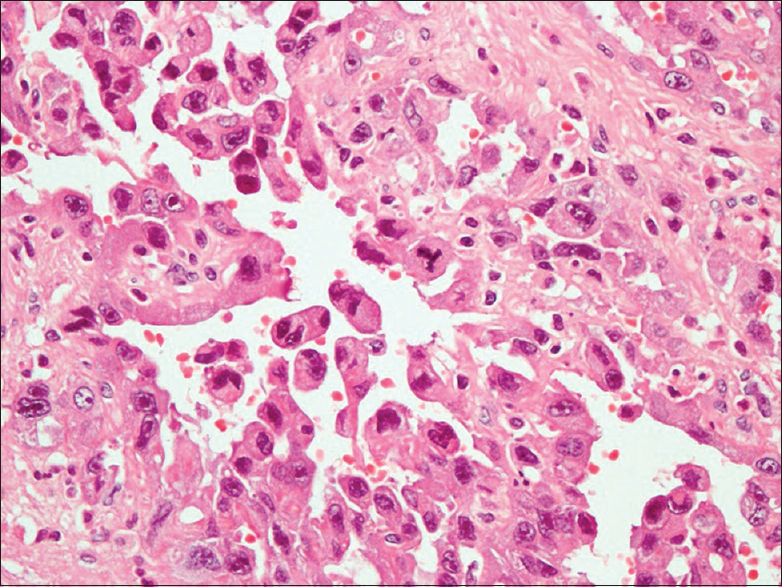 | Figure 3: Immunohistochemistry - CD 31 - positive staining of atypical endothelial cells
Click here to view |
In view of high-grade malignancy, whole body positron emission tomography-computed tomography was done, which revealed liver metastasis for which liver biopsy was done, which revealed angiosarcoma. The patient was given postoperative chemotherapy, but the patient died after 6 months of treatment due to distant metastasis.
 Discussion Discussion | |  |
Though rare but benign tumors have the potential for malignant transformation.[1],[2] Angiosarcoma transformation in peripheral nerve sheath tumors is rare. Usually such tumors transform into neurofibromas or malignant peripheral nerve sheath tumors, especially in von reckinghausen disease.[3],[4] The process of malignant transformation from schwannoma to angiosarcoma was postulated by Rückert et al.[1] Although FNA is clearly a good diagnostic tool that can be performed easily in the outpatient clinic once the mass had completely changed to malignant cells, FNA for diagnosis of schwannoma is difficult and the accuracy reported was only 20%.[5],[6] Sometimes it is difficult to detect the earlier malignant transformation even by FNA. Thus, our physicians should be cognizant of the need for careful follow-up including MRI and FNA of benign neurogenic tumors of the neck because of this potential for transformation. Recently, a new case of malignant transformation to angiosarcoma is very interestingly discussed.[7] The accumulation of more cases in the literature will help physicians decide on future diagnostic and treatment strategies.
 Conclusion Conclusion | |  |
Because neurogenic tumors sometimes undergo malignant transformation, we recommend that for neck masses suspected to be benign, surgery should be performed if possible. However, if follow-up observation is chosen, MRI and FNA should be regular, and patients should sign a statement acknowledging awareness of the potential for malignant transformation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
 References References | |  |
| 1. | Rückert RI, Fleige B, Rogalla P, Woodruff JM. Schwannoma with angiosarcoma. Report of a case and comparison with other types of nerve tumors with angiosarcoma. Cancer 2000;89:1577-85.  |
| 2. | Li C, Chen Y, Zhang H, Zheng X, Wang J. Epithelioid angiosarcoma arising in schwannoma: Report of three Chinese cases with review of the literature. Pathol Int 2012;62:500-5.  |
| 3. | Elli M, Can B, Ceyhan M, Pinarli FG, Dagdemir A, Ayyildiz HS, et al. Intrathoracic malignant peripheral nerve sheath tumor with angiosarcoma in a child with NF1. Tumori 2007;93:641-4.  |
| 4. | Mentzel T, Katenkamp D. Intraneural angiosarcoma and angiosarcoma arising in benign and malignant peripheral nerve sheath tumours: Clinicopathological and immunohistochemical analysis of four cases. Histopathology 1999;35:114-20.  |
| 5. | Yu GH, Sack MJ, Baloch Z, Gupta PK. Difficulties in the fine needle aspiration (FNA) diagnosis of schwannoma. Cytopathology 1999;10:186-94.  |
| 6. | Liu HL, Yu SY, Li GK, Wei WI. Extracranial head and neck schwannomas: A study of the nerve of origin. Eur Arch Otorhinolaryngol 2011;268:1343-7.  |
| 7. | Ogawa T, Kato T, Ikeda A, Nishimura K, Tsuchiya Y, Okamoto H, et al. Case of malignant transformation of vagus nerve schwannoma to angiosarcoma. Head Neck 2014;36:E17-20.  |
[Figure 1], [Figure 2], [Figure 3]
|