|


 |
| ORIGINAL ARTICLE |
|
| Year : 2015 | Volume
: 7
| Issue : 2 | Page : 32-36 |
|
|
Acute physiological and chronic health evaluation ii score and its correlation with three surgical strategies for management of ileal perforations
Anand Munghate1, Ashwani Kumar1, Sushil Mittal1, Harnam Singh1, Jyoti Sharma2, Manish Yadav1
1 Department of Surgery, Government Medical College, Patiala, Punjab, India
2 Department of Pathology, Pandit Bhagwan Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India
| Date of Web Publication | 6-Jul-2016 |
Correspondence Address:
Anand Munghate
Department of Surgery, Government Medical College, Patiala - 147 001, Punjab
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2006-8808.185653

 Abstract Abstract | | |
Introduction: Ileal perforation peritonitis is a common surgical emergency in the Indian subcontinent and in tropical countries. It is reported to constitute the fifth common cause of abdominal emergencies due to high incidence of enteric fever and tuberculosis in these management based on Acute Physiological and Chronic Health Evaluation II (APACHE II) score. Methods: The following study was conducted in the Department of General Surgery, Government Medical College, Patiala. A total of 57 patients were studied and divided in to Group I, II, and III. APACHE II score accessed and score between 10 and 19 were blindly randomized into three procedures primary closure, resection-anastomosis, and ileostomy. The outcome was compared. Results: Ileal perforations were most commonly observed in the third and fourth decade of life with male dominance. APACHE II score was accessed and out of total 57 patients, 6 patients had APACHE II score of 0-9, 48 patients had APACHE II score of 10-19, and 3 patients had APACHE II score of ≥20. In APACHE II score 10-19, 15 patients underwent primary closure, 16 patients underwent resection-anastomosis, and 17 patients underwent ileostomy. Discussion and Conclusion: Primary closure of perforation is advocated in patients with single, small perforation (<1 cm) with APACHE II score 10-19 irrespective of duration of perforation. Ileostomy is advocated in APACHE II score 10-19, where the terminal ileum is grossly inflamed with multiple perforations, large perforations (>1 cm), fecal peritonitis, matted bowel loops, intraoperative evidence of caseating lymph nodes, strictures, and an unhealthy gut due to edema. Keywords: Acute abdomen, Acute Physiological and Chronic Health Evaluation II, ileostomy, intestinal perforation, peritonitis
How to cite this article:
Munghate A, Kumar A, Mittal S, Singh H, Sharma J, Yadav M. Acute physiological and chronic health evaluation ii score and its correlation with three surgical strategies for management of ileal perforations. J Surg Tech Case Report 2015;7:32-6 |
How to cite this URL:
Munghate A, Kumar A, Mittal S, Singh H, Sharma J, Yadav M. Acute physiological and chronic health evaluation ii score and its correlation with three surgical strategies for management of ileal perforations. J Surg Tech Case Report [serial online] 2015 [cited 2018 Jul 1];7:32-6. Available from: http://www.jstcr.org/text.asp?2015/7/2/32/185653 |
 Introduction Introduction | |  |
Ileal perforation peritonitis is a common surgical emergency in Indian subcontinent and in tropical countries. It is reported to constitute the fifth common cause of abdominal emergencies due to high incidence of enteric fever and tuberculosis in these regions. Despite the availability of modern diagnostic facilities and advances in treatment regimes, this condition is still associated with a high morbidity and mortality. [1],[2]
Surgical approach is the standard treatment of ileal perforations and is the only successful modality, but the choice of procedure continues to be debated. Various strategies are being used to deal with ileal perforations including primary closure of perforation with or without omental patch, repair of perforation with ileotransverse colostomy, ileostomy, exteriorization, trimming of ulcer edge and closure, wedge excision and anastomosis, and segmental resection and anastomosis. [3]
Severity scoring is a valuable tool for assessing and quantification of severity of acute illness. Currently Acute Physiological and Chronic Health Evaluation (APACHE II) scoring system is the best available method for risk stratification in abdominal sepsis. In our study, we have compared different surgical procedures for ileal perforation using APACHE II score and what procedure was suitable in different groups of patients with different APACHE II scores.
The proposed study aims to compare and contrast three different surgical approaches to ileal perforation management, i.e. simple closure, resection, and anastomosis and ileostomy, to define the severity of peritonitis based on APACHE II score in cases of ileal perforation, identify the cause, define the criteria for choosing a particular modality of treatment and compare the short- and long-term outcome of the various treatment modalities.
The study will help to establish the criteria for instituting the management modality according to presentation and severity of the disease and the outcome of these procedures. Effective management of the disease will help in decreasing morbidity and mortality associated with the disease.
 Methods Methods | |  |
The following study was conducted in the Department of General Surgery, Government Medical College and Rajindra Hospital, Patiala, on patients who were admitted from casualty and surgical outpatient department from July 2012 to October 2013 with a proven diagnosis of ileal perforation peritonitis. A total of 57 patients were studied and divided in to following groups, Group I: These patients were managed by primary repair of the perforation. Group II: These patients were managed by resection-anastomosis, and Group III: These patients were managed by ileostomy with closure/resection of perforation. Inclusion and exclusion criteria were decided.
Inclusion criteria
- All cases of perforation peritonitis with strong suspicion of small bowel perforation (ileal) without any prior diagnosis of any pathology
- Patients belonging to Group II according to APACHE II score.
Exclusion criteria
- Previous diagnosis of intestinal tuberculosis
- Children below 12 years
- Pregnant females
- Renal, hepatic, rheumatic, or vascular disease
- Patients lost to follow-up.
Detailed history, complete general physical examination, selection of patients into groups by APACHE II scoring, and investigations were noted from the patients in the study group. The patients were divided into study groups based on their APACHE II scores - Group I: 0-9, Group II: 10-19, Group III: ≥20. Patients with APACHE II score between 10 and 19 were blindly randomized into three procedures primary closure, resection-anastomosis, or ileostomy.
Acute Physiology and Chronic Health Evaluation II
A: Physiological variables to be studied and analyzed by Acute Physiology and Chronic Health Evaluation II
Temperature, mean arterial pressure (mm Hg), heart rate (per min), respiratory rate (per min), pH, PaO 2 , sodium (mmol/l), potassium (mmol/l), creatinine (mg%), hematocrit (%), white blood cell count (/cumm), Glasgow coma scale.
B: Age points
- <44 years = 0
- 45-54 years = 2
- 55-64 years = 3
- 65-74 years = 5
- >75 years = 6.
C: Chronic health points
Nonoperative or emergency postoperative +5 points, elective postoperative +2 points.
APACHE II score = A + B + c.
Outcome was assessed by the number and duration of hospital stay, wound infection, wound dehiscence, leakage/fecal fistula, intra-abdominal collections/abscesses, ileostomy related complications (output; fluid and electrolyte imbalance; retraction; stenosis), and reoperation(s). The study concluded when the patient recovered fully or the patient expired, and the patients were followed up till 30 days from the date of admission. Those with ileostomy were followed up till the ileostomy was closed and for a further period of 2 weeks in case of complications. Patients lost to follow-up were excluded from the study.
 Results Results | |  |
During the 15 months period of study, ileal perforations were most commonly observed in third and fourth decade of life with males more commonly affected (male:female 1.85:1). Abdominal pain was the most common clinical presentation (100%) followed by fever, abdominal distension, vomiting, and obstipation. The etiology of perforation was typhoid (38.59%), nonspecific (36.84%), tuberculosis (14.03%), and trauma (10.52%). Majority of the patients presented within 48 h of perforation (73.68%) [Table 1].
APACHE II score was accessed and out of total 57 patients, 6 (10.52%) patients had APACHE II score 0-9, 48 patients (84.21%) had APACHE II score 10-19, and 3 patients (5.26%) had APACHE II score ≥20. In APACHE II score 10-19, 15 patients (31.25%) underwent primary closure, 16 patients (33.33%) underwent resection-anastomosis, and 17 patients (35.41%) underwent ileostomy [Table 2]. Complications in all the procedures were noted and resulted that wound infection was the most common complication (71.92%). It was present in about 75% cases each in patients having undergone primary closure of perforation and resection-anastomosis for ileal perforation peritonitis as compared to about 66.66% in patients having undergone ileostomy [Table 3]. Morbidity was found more in Group III, which was related to ileostomy related complications (P < 0.05). One patient each in Groups II and III expired accounting for mortality [Table 4].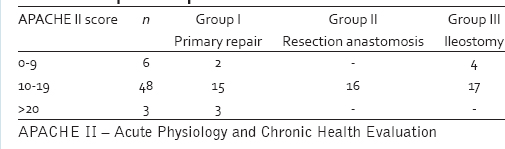 | Table 2: Acute Physiology and Chronic Health Evaluation II score and operative procedure
Click here to view |
 Discussion Discussion | |  |
Nontraumatic perforation of the small intestine is one of the common surgical emergencies encountered by surgeons in developing countries. Surgery is the ideal treatment as it eliminates soiling of peritoneal cavity in an effort to lessen the toxemia and enhance the recovery of the patient. However, there is no uniformity of standardized operative procedure that is most effective for the offending lesion.
There are also no criteria which define the type of surgical procedure based on the sepsis score. In the present study, all the patients were scores according to the APACHE II score. It was decided that patients with APACHE II score <9 would undergo primary closure of the perforation since the general condition of the patient and the associated peritonitis were conducive to good healing. In patients with APACHE II score ≥20, the policy was to form a ileostomy proximal to the perforation(s), since primary repair in advanced stages of peritonitis in patients with poor general conditions would most likely lead to higher incidence of local complications. The present study in patients with APACHE II score 10-19 aimed to establish whether primary closure of the perforation and formation of a proximal ileostomy would be the best treatment of choice.
Small bowel perforations most commonly affect the young in the prime of their life. In the present study, male preponderance was found with male to female ratio of 1.85:1 that is slightly on the lower side of the ratio 3:1 reported by Wani et al., 4:1 reported by Adesunkanmi et al. and Talwar et al. [4],[5],[6]
In the present study, different operative procedures - simple closure of perforation, resection-anastomosis, and ileostomy were performed according to cause and severity of illness. Simple closure was done in 20 patients, 15 of which had APACHE II score 10-19. These patients had single perforation, small in size (≤1 cm), located within 60 cm of ileum with less peritoneal contamination. In 16 patients, resection anastomosis was performed, 15 of which had APACHE II score 10-19. Resection-anastomosis was performed because of multiple perforations or large perforation (>2 cm) or when segment of bowel appeared unhealthy for simple closure. In the literature, simple closure is recommended for single perforations with less peritoneal contamination, [2],[6],[7],[8],[9] while wedge excision, segmental resection and anastomosis, ileotransverse anastomosis have been recommended for multiple perforations, diseased segment of bowel. [2],[10],[11],[12],[13]
Primary closure of perforation was done in 13 patients with single perforation of size <1 cm. The complication rate was 46.6%. Seven patients with large perforation also underwent primary closure. The complication rate in them was 85.71%. Resection-anastomosis was done in 16 patients, 5 out of which had large perforations (>1 cm). The complication rate was 75%. The morbidity associated with primary closure is 75% which is less than the morbidity of 80.9% and 52.3% associated with ileostomy formation and closure, respectively (P < 0.05). Simple repair of perforation in two layers is the treatment of choice for typhoid perforation. Two layer closure of the perforation with or without an omental patch has been most successful. [8] Surgical management with primary closure of the perforation (74.5%), closure with omental graft (14.5%), resection and anastomosis (3.6%), and only drainage (7.3%) was done by Talwar et al. The morbidity rate was 79.1% and mortality rate was 16.4%. The mortality was least with early primary closure of perforation. [6]
If there are multiple perforations and any area of bowel seems unhealthy or liable to perforate, a length of small bowel should be resected, including all the diseased part and a two layer anastomosis is performed. Mortality rates were 43% for ileostomy, 36% for primary closure, 15% for those treated with wedge resection. [14] Shah et al. observed that it is better to opt for resection-anastomosis irrespective of the number of perforations and found lower complication rate (35.5%) and mortality rate (21.47%) in comparison to simple closure complication rate (71.25%) and mortality rate (42.96%) to ileostomy complication rate (100%) and mortality rate (77.77%). Pal reported 6.22% mortality with simple closure and ileotransverse anastomosis and found it to be better. [15]
Ileostomy was performed in 21 patients, 10 of which had APACHE II score 10-19. Ileostomy was recommended in cases of poor general condition, extensive contamination, perforation situated near the ileocecal junction, large perforations (>1 cm), intraoperative findings suggestive of strictures, caseating lymph nodes. In 17 patients with single, small perforation (<1 cm), ileostomy was made depending upon high APACHE II score, extensive fecal contamination, unhealthy bowel wall. The complication rate was 56.2%. About 5 patients with large perforations (>1 cm) and 4 patients with multiple perforations underwent ileostomy formation. The complication rate in them was observed to be 62.5%. Mortality was more in patients with multiple perforations as compared to single perforation (P < 0.025). Development of fecal fistula was unrelated to number of perforations. [16]
Closure of the perforation combined with ileotransverse colostomy was found to have a definite improvement in recovery, mortality reduced from 75% to 20%. [11] Eggleston observed mortality was same but morbidity decreased (P < 0.02) with closure of perforation and ileotransverse colostomy; this takes the diseased bowel out of the intestinal mainstream. [17] Extensive procedures such as resection-anastomosis and right hemicolectomy should be avoided in patients with poor general condition and toxemia. Ileostomy as a secondary procedure should be considered once fecal fistula develops in order to avoid peritoneal contamination. The mortality is unrelated to the duration of perforation and the type of operation performed (P < 0.05). [18]
Wound infection was the most common postoperative complication-about 75% each in Groups I and II, followed by intra-abdominal collections, wound dehiscence, and anastomotic leak, which is in accordance with previous studies (P < 0.05). [4],[5],[15],[16] The other complications in Group II were related to ileostomy which hampered quality of life and significantly added to morbidity in these patients.
The average APACHE II score in Group I was 14.95, Group II was 12.375 and was 12.285 Group III. Patients with APACHE II score 10-19 had 73.0% morbidity and mortality 7.6% as compared to 38.7% in those having APACHE II score 0-9. No mortality occurred in patients with APACHE II score 0-9. Two deaths occurred in those with APACHE II score 10-19, one was diagnosed typhoid perforation in an old male, and other was nonspecific perforation in adult female. Chest infection, renal failure, and sepsis accounted for their mortality. One patient with APACHE II score 21 managed to survive. Studies have reported unfavorable outcome in patients with APACHE II score of 20 or greater. High APACHE II score has predicted prognosis and mortality in various studies. [19],[20],[21] APACHE II score predicted postoperative mortality in the study by Adesunkanmi et al. However, its ability to predict postoperative morbidity was not confirmed. In our study high score related to high morbidity as well. [5]
 Conclusion Conclusion | |  |
Primary closure of perforation is advocated in patients with single, small perforation (<1 cm) with APACHE II score 10-19 irrespective of duration of perforation. Ileostomy is advocated in APACHE II score 10-19, where the terminal ileum is grossly inflamed with multiple perforations, large perforations (>1 cm), fecal peritonitis, matted bowel loops, intraoperative evidence of caseating lymph nodes, strictures, and an unhealthy gut due to edema. The repair of perforation has been advocated as better procedure than temporary ileostomy due to its cost effectiveness, absence of complications related to ileostomy, and the need for second surgery for ileostomy closure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
 References References | |  |
| 1. | Siddiqui S. Epidemiologic patterns and control strategies in typhoid fever. J Pak Med Assoc 1991;41:143-6.  |
| 2. | Pal DK. Evaluation of best surgical procedures in typhoid perforation - An experience of 60 cases. Trop Doct 1998;28:16-8.  |
| 3. | Farooq T, Rashid MU, Lodhi M, Farooq A, Ahmad S. Enteric ileal perforation primary repair versus loop ileostomy. APMC 2011;5:15-8.  |
| 4. | Wani RA, Parray FQ, Bhat NA, Wani MA, Bhat TH, Farzana F. Nontraumatic terminal ileal perforation. World J Emerg Surg 2006;1:7.  |
| 5. | Adesunkanmi AR, Badmus TA, Fadiora FO, Agbakwura EA. Generalised peritonitis secondary to typhoid ileal perforation. Assessment of severity using modified APACHE II score. Indian J Surg 2005;67:29-33.  |
| 6. | Talwar S, Sharma RK, Mittal DK, Prasad P. Typhoid enteric perforation. Aust N Z J Surg 1997;67:351-3.  |
| 7. | Eggleston FC, Santoshi B, Singh CM. Typhoid perforation of the bowel. Experiences in 78 cases. Ann Surg 1979;190:31-5.  |
| 8. | Khanna AK, Misra MK. Typhoid perforation of the gut. Postgrad Med J 1984;60:523-5.  |
| 9. | Kim JP, Oh SK, Jarrett F. Management of ileal perforation due to typhoid fever. Ann Surg 1975;181:88-91.  |
| 10. | Dickson JA, Cole GJ. Perforation of the terminal ileum. A review of 38 cases. Br J Surg 1964;51:893-7.  |
| 11. | Prasad PB, Choudhury DK, Prakash O. Typhoid perforation treated by closure and proximal side to side ileotransverse colostomy. J Indian Med Assoc 1975;65:297-9.  |
| 12. | Ameh EA, Dogo PM, Attah MM, Nmadu PT. Comparison of three operations for typhoid perforation. Br J Surg 1997;84:558-9.  |
| 13. | Saxe JM, Cropsey R. Is operative management effective in treatment of perforated typhoid? Am J Surg 2005;189:342-4.  |
| 14. | Welch TP, Martin NC. Surgical treatment of typhoid perforation. Lancet 1975;1:1078-80.  |
| 15. | Shah AA, Wani KA, Wazir BS. The ideal treatment of the typhoid enteric perforation - Resection anastomosis. Int Surg 1999;84:35-8.  |
| 16. | Adesunkanmi AR, Ajao OG. The prognostic factors in typhoid ileal perforation: A prospective study of 50 patients. J R Coll Surg Edinb 1997;42:395-9.  |
| 17. | Eggleston FC, Santoshi B. Typhoid perforation: Choice of operation. Br J Surg 1981;68:341-2.  |
| 18. | Beniwal U, Jindal D, Sharma J, Jain S, Shyam G. Comparative study of operative procedures in typhoid perforation. Indian J Surg 2003;65:172-7.  |
| 19. | Siddiqui G, Sheikh JM, Soomro AG. Outcome of ileostomy in management of ileal perforation. JLUMHS 2008;7:168-72.  |
| 20. | Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: A physiologically based classification system. Crit Care Med 1981;9:591-7.  |
| 21. | Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med 1985;13:818-29.  |
[Table 1], [Table 2], [Table 3], [Table 4]
|