|


 |
| CASE REPORT |
|
| Year : 2015 | Volume
: 7
| Issue : 2 | Page : 48-50 |
|
|
Echinococcal cyst of the pancreas with Cystopancreatic duct fistula successfully treated by partial cystectomy and Cystogastrostomy
Ahmed Elaffand1, Adarsh Vijay2, Samah Mohamed1, Hassan Hani Al-Battah2, Ayda Youssef1, Ahmed Farahat1
1 National Cancer Institute, Cairo, Egypt
2 Hamad Medical Corporation, Doha, Qatar
| Date of Web Publication | 6-Jul-2016 |
Correspondence Address:
Ahmed Elaffand
Department of Surgical Oncology, National Cancer Institute, Cairo University, Cairo
Egypt
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2006-8808.185657

 Abstract Abstract | | |
The primary pancreatic hydatid (echinococcal) cyst is extremely rare with a reported incidence of <1%. Owing to its rareness and a considerable overlap of imaging features, a preoperative diagnosis is usually difficult. The dilemma in confirming this benign diagnosis has often questioned the extent of radical pancreatic resection. The involvement of pancreatic duct (cystopancreatic duct fistula) further complicates the management of such cystic lesions. In this report, we present a case of isolated hydatid cyst of the pancreatic body and tail communicating with the pancreatic duct. Cystogastrostomy preceded by partial cystectomy in the same setting has never been reported to date. The patient had an uneventful postoperative course and follow-up showed no evidence of cyst recurrence or dissemination. We consider this a safe surgical option in longstanding large cysts, especially if a cystopancreatic fistula is detected beforehand. The success of such a procedure however may rely on the size and thickness of the cyst wall to support this anastomosis. Keywords: Echinococcal cyst pancreas cystogastrostomy, Hydatid pancreas cystogastrostomy
How to cite this article:
Elaffand A, Vijay A, Mohamed S, Al-Battah HH, Youssef A, Farahat A. Echinococcal cyst of the pancreas with Cystopancreatic duct fistula successfully treated by partial cystectomy and Cystogastrostomy. J Surg Tech Case Report 2015;7:48-50 |
How to cite this URL:
Elaffand A, Vijay A, Mohamed S, Al-Battah HH, Youssef A, Farahat A. Echinococcal cyst of the pancreas with Cystopancreatic duct fistula successfully treated by partial cystectomy and Cystogastrostomy. J Surg Tech Case Report [serial online] 2015 [cited 2018 Jul 1];7:48-50. Available from: http://www.jstcr.org/text.asp?2015/7/2/48/185657 |
 Introduction Introduction | |  |
Hydatid disease (HD) is a rare endemic disease in many countries that may affect any organ or tissue. The most common site being the liver (59-75%), followed in frequency by lung (27%), kidney (3%), bone (1-4%), and brain (1-2%). [1],[2],[3] Isolated involvement of the pancreas is unusual, accounting for <1% of the cases (mostly reported in the head of the pancreas). [4] Medical therapy is a preferable choice in small lesions, however partial cystectomy and limited pancreatic resection have been reported in larger cysts. [3] The presence of a cystopancreatic fistula may cause a long-lasting pancreatic leak after fenestration of large hydatid cysts. [3] There is still a limited knowledge on the best surgical approach in the management of large hydatid cysts involving the pancreatic duct.
 Case report Case report | |  |
A 34-year-old male presented to the outpatient clinic at the National Cancer Institute, Cairo University with epigastric swelling, upper abdominal pain, and vomiting for 3 days. On clinical examination, an epigastric mass (8 cm × 10 cm) was palpable. Biochemical laboratory investigations showed raised C-reactive protein (46 mg/L). All other investigations were within normal limits including pancreatic amylase, carcinoembryonic antigen (CEA), and CA 19-9. Initial imaging (liver ultrasound and chest/abdominal X-ray) showed a large epigastric swelling 11 cm × 8 cm that was closely related to the pancreas.
Magnetic resonance imaging (MRI) of the pancreas revealed a well-defined rounded cystic lesion abutting the ventral portion of the central pancreas. The cyst wall thickness measured 7 mm. Multiple low signal intracystic strands were noted floating within, associated with a distinctive hypointense ring of the pericystic lining. No daughter cysts could be seen indicating that the cyst can be classified CE Type 3 a (transitional hydatid cyst) as per the WHO Informal Working Group classification. [5] The pancreatic duct was seen as a hyperintense line leading to the lesion [Figure 1]. Consequently, HD was confirmed with a positive indirect hemagglutination test.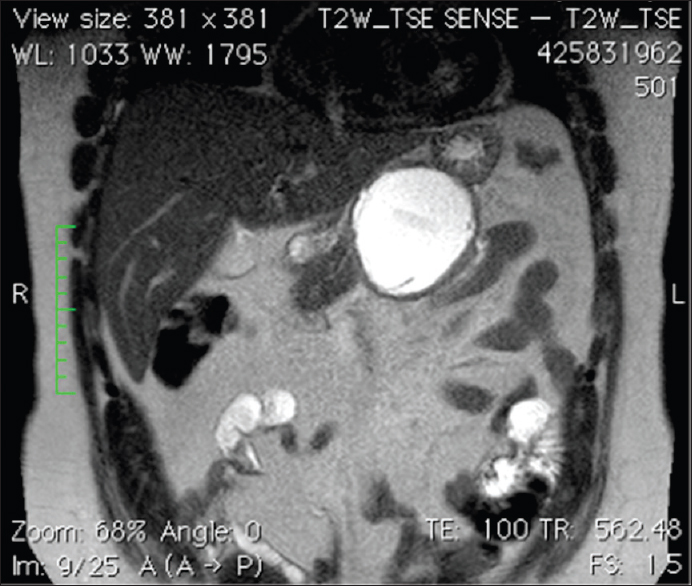 | Figure 1: Coronal T2-weighted image of the pancreas showing a well-defined rounded cystic lesion abutting the ventral portion of the central pancreas. No daughter cysts could be seen indicating that the cyst is a Type CE 3 a (transitional hydatid cyst). The pancreatic duct is seen (as hyperintense line) leading to the lesion
Click here to view |
A diagnosis of isolated HD of the pancreas was made and the case was discussed at the hepatopancreaticobiliary multidisciplinary team meeting, and all members approved a surgical plan for partial cystectomy and cystogastrostomy due to pancreatic duct involvement. The patient was started initially for a month at a high dose of albendazole (800 mg/day). His liver functions were checked 2 weeks into the course and were completely normal. He then spent 2 weeks free of medical therapy before resuming his second course at the same dose for a month before surgery.
Surgical exploration revealed a large cyst involving the body and tail of the pancreas densely adherent to the adjacent stomach and transverse colon. The rest of the abdominal cavity was free with no evident HD of the liver or spleen. The anterior wall of the stomach was opened. The surgical area was protected with a scolicidal solution to prevent any intra-abdominal dissemination. Posterior wall of the stomach was incised following injection of hypertonic saline. Partial cystectomy was carried out to access the cyst cavity and evacuate it completely along with argonizing the inner lining of the cyst before joining the cyst to the stomach with continuous polydioxanone suture to fashion a posterior cystogastrostomy. The anterior gastrostomy was closed in two layers. Postoperative confirmation of the hydatid cysts was obtained on the basis of the histopathological findings. Both fluid cytology and tissue pathology were negative for any malignant changes and confirmed good response to medical therapy. The patient had an uneventful postoperative course and was discharged on albendazole 800 mg/day for a period of 3 months. At 1 year follow-up, clinical examination, abdominal ultrasonography, and indirect hemagglutination tests showed no evidence of cyst recurrence or dissemination.
 Discussion Discussion | |  |
HD is a parasitic disease most commonly caused by the larval stage of Echinococcus granulosus. Humans serve as intermediate hosts and are affected by hydatidosis. The mode of infestation is either hematogenous or more rarely lymphatic. [6] HD of the pancreas is rare (<1%) compared to the other sites of HD. [7]
Despite technological advancement, diagnosis of hydatid cysts remains challenging. The serological and immunological tests vary in their sensitivity. Abdominal ultrasound has shown a diagnostic accuracy close to 95% in recent studies. [8] However, a high index of suspicion is mandated in such rare pancreatic pathologies, especially in endemic areas. MRI, due to its higher soft tissue contrast and multiplanar capability, helps characterize the cyst, differentiate cystic neoplasms, and provides its relation to pancreatic duct. [9] In our case, the hydatid cyst was radiologically classified as "transitional" before the commencement of medical antihelminthic therapy, which contradicts the existence of positive serology at the same time. We speculate that such an effect might have been due to the presence of cystopancreatic fistula and exposure of the cyst contents to the digestive pancreatic enzymes. Cytology of the cyst fluid or biopsy of the cystic wall are indeed useful in doubtful/borderline cases; however, the preoperative images with a positive hydatid serology and negative CEA provided a `reliable high degree of evidence that the patient was having a hydatid cyst of the pancreas that was communicating with the pancreatic duct. Furthermore, the concern of spillage of hydatid cyst contents into the peritoneum precluded the use of such invasive diagnostic modalities.
Surgical treatment of hydatid pancreatic cysts is not well described in literature due to the rare nature of this disease. Medical therapy with albendazole is preferable if small cysts are encountered; however, the treatment varies if larger segments of the pancreas are involved. [7] Surgical treatment of the diseased pancreatic segment depends on its location, and may vary from cyst fenestration to segmental resection. [4],[5],[6],[7] Cystopancreatic fistula may cause a long-lasting pancreatic leak after fenestration and therefore a definitive (resection) treatment is preferred if such a fistula is detected before surgery. [3] However, definitive resection may lead to higher morbidity rates and is feasible only in select patients meeting the criteria in the location of the cyst and its relationship to other vital anatomical structures. [10] Alternative limited surgical options have rarely been described to date.
Although existing literature would support a total cystopericystectomy ± omentoplasty for pancreatic hydatid cysts not restricted to the tail, our HPB Committee concern toward such an approach was the communication of the hydatid cyst with the pancreatic duct which to the authors' view may have led to postoperative pancreatic fistula.
Cystogastrostomy preceded by partial cystectomy in the same setting has never been reported in literature as a surgical management for pancreatic hydatid cyst with pancreatic duct involvement. We consider this a safe surgical option in longstanding large cysts, especially if a cystopancreatic fistula is detected beforehand. The success of such a procedure however may rely on the size and thickness of the cyst wall to support this anastomosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
 References References | |  |
| 1. | Yuksel M, Demirpolat G, Sever A, Bakaris S, Bulbuloglu E, Elmas N. Hydatid disease involving some rare locations in the body: A pictorial essay. Korean J Radiol 2007;8:531-40.  |
| 2. | Geramizadeh B. Unusual locations of the hydatid cyst: A review from Iran. Iran J Med Sci 2013;38:2-14.  |
| 3. | Bedioui H, Chebbi F, Ayadi S, Daghfous A, Bakhtri M, Jouini M, et al. Primary hydatid cyst of the pancreas: Diagnosis and surgical procedures. Report of three cases. Gastroenterol Clin Biol 2008;32(1 Pt 1):102-6.  |
| 4. | Makni A, Jouini M, Kacem M, Safta ZB. Acute pancreatitis due to pancreatic hydatid cyst: A case report and review of the literature. World J Emerg Surg 2012;7:7.  |
| 5. | WHO Informal Working Group. International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop 2003;85:253-61.  |
| 6. | Dziri C. Hydatid disease - continuing serious public health problem: Introduction. World J Surg 2001;25:1-3.  |
| 7. | Moosavi SR, Kermany HK. Epigastric mass due to a hydatid cyst of the pancreas. A case report and review of the literature. JOP 2007;8:232-4.  |
| 8. | Balik AA, Celebi F, Basglu M, Oren D, Yildirgan I, Atamanalp SS. Intra-abdominal extrahepatic echinococcosis. Surg Today 2001;31:881-4.  |
| 9. | Xiao B, Zhang XM, Tang W, Zeng NL, Zhai ZH. Magnetic resonance imaging for local complications of acute pancreatitis: A pictorial review. World J Gastroenterol 2010;16:2735-42.  |
| 10. | Wronski M, Slodkowski M, Cebulski W, Moronczyk D, Krasnodebski IW. Optimizing management of pancreaticopleural fistulas. World J Gastroenterol 2011;17:4696-703.  |
[Figure 1]
|