|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2013 | Volume
: 15
| Issue : 1 | Page : 7-12 |
|
A Descriptive Study of Clefts of the Primary and Secondary Palate Seen in a Tertiary Institution in Nigeria
A Ibrahim1, PM Mshelbwala2, AC Obiadazie3, CN Ononiwu3, ME Asuku1, SO Ajike3, EA Ameh2
1 Department of Surgery; Division of Plastic Surgery, Ahmadu Bello University, Zaria, Nigeria
2 Department of Surgery; Division of Pediatric, Surgery Ahmadu Bello University, Zaria, Nigeria
3 Department of Maxillofacial Surgery, Ahmadu Bello University, Zaria, Nigeria
| Date of Web Publication | 22-Sep-2014 |
Correspondence Address:
A Ibrahim
Department of Surgery, Division of Plastic Surgery, Ahmadu Bello University, Zaria
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/1595-1103.141384

Background: Cleft lip and palate is the commonest congenital malformation of the head and neck region. This article discusses the experiences of the authors' in the management of clefts of the primary and secondary palate in a tertiary institution in Nigeria.
Patients and Methods: This is a retrospective review of the clinical database for all children with cleft lip and palate. Data were analyzed for age at presentation, sex distribution, surgical technique, associated congenital anomalies, and complications. The results obtained were converted to relative values in frequency tables for analysis.
Results: The average age at presentation for all patients with cleft was 2.47 years. Males were slightly more affected than females among all clefts with a frequency of 40 (53%) and 35 (47%). The distribution of clefts by location showed a preponderance of the left side 33 (44%), followed by right side 18 (24%) and bilateral cases 11 (15%). Three patients (4%) had a relative with a cleft of the primary or secondary palate. At least one congenital malformation coexisted with a cleft of the primary or secondary palate in 13 (17%) of the 75 babies. The commonest post-operative complication of cleft of the primary palate was wound dehiscence 3 (4%).
Conclusion: This study has shown that there was a wide range of age at presentation. It is characterized by delays in the repair of clefts of the primary and secondary palate. We strongly support early repair of clefts of the primary and secondary palate to facilitate normal feeding, better speech and ensure social acceptance. Keywords: Cleft, late presentation, Millard′s repair, primary palate, secondary palate, von Langenbeck′s technique
How to cite this article:
Ibrahim A, Mshelbwala P M, Obiadazie A C, Ononiwu C N, Asuku M E, Ajike S O, Ameh E A. A Descriptive Study of Clefts of the Primary and Secondary Palate Seen in a Tertiary Institution in Nigeria. Niger J Surg Res 2013;15:7-12 |
How to cite this URL:
Ibrahim A, Mshelbwala P M, Obiadazie A C, Ononiwu C N, Asuku M E, Ajike S O, Ameh E A. A Descriptive Study of Clefts of the Primary and Secondary Palate Seen in a Tertiary Institution in Nigeria. Niger J Surg Res [serial online] 2013 [cited 2017 Jan 22];15:7-12. Available from: http://www.njsrjournal.org/text.asp?2013/15/1/7/141384 |
| Introduction | |  |
Cleft lip and palate is the commonest congenital malformation of the head and neck region. [1] Its appearance is heralded by a unique set of physical abnormalities leading to impairments of speech, hearing, and dental development. It is also accompanied by aesthetic anomalies which compound the stigma of the condition and negatively impact upon the psychosocial development of affected individuals and their families. [2] Given the detrimental effects on physical and psychological well being, a comprehensive approach in the management of cleft lip and palate has received significant attention in the surgical literature over the last half century. [3],[4] The accepted and current standard of care is a multidisciplinary approach. Periodic evaluation of the patient, good supportive care, close and rigorous follow-up, and adherence to the established time scale are important components for a successful outcome. [5] A wide range of clefts' treatment protocols exists but the ideal surgical technique and timing protocol is a subject of ongoing debate. [3]
In most developed countries, children born with cleft lip and palate are usually seen at or very shortly after birth, often by a team comprising a pediatrician, plastic surgeon, oral surgeon, orthodontist, speech therapist, pediatric nurse, prosthodontist, otorhinolaryngologist, and anesthetist. Early contact with the baby and parents by the cleft team, allows timely repair of both lip and palate with subsequent expert orthodontics and speech therapy, thereby ensuring good functional and aesthetic outcome. [6] Such an optimum approach is impossible in many developing countries including Nigeria. [7],[8],[9] Studies have shown that interdisciplinary care for the cleft patient is not yet fully embraced in Africa and team care is perhaps many years behind the global trend. [4],[6],[10] This may be a result of several reasons including the relatively young age of cleft care practice and a lack of specialists. [10] Furthermore, lack of awareness of treatment availability, superstition, and lack of money contribute to late or non-presentation for surgery. [4] Many patients are thus not seen early, with a significant number presenting for the first time in late childhood and, in some instances, in adults above the age of 35 years. [6] Thus, both attempts to provide standards of care for these patients and analysis of clinical data in relation to these standards from low resource settings remain valuable. [3] This report discusses the epidemiology and clinical profile of clefts of the primary and secondary palate in a tertiary institution in Nigeria.
| Patients and Methods | |  |
We conducted a retrospective review of the clinical database for all children with cleft lip and palate treated at Ahmadu Bello University Teaching Hospital Zaria from June 2002 to November 2013. The center consists of a team of cleft surgeons (two plastic surgeons, two pediatric surgeons, and four maxillofacial surgeons).
A detailed assessment of the patients' by the cleft team is performed at the cleft clinic. A medical history is recorded including pregnancy history, associated congenital anomalies, and a family history. Clinical photographs are routinely obtained in all the patients and a classification of the cleft is made. [Figure 1]a, [Figure 2]a, and [Figure 3]a. The classification employed was that of Kernahan and Stark's. [11] Clefts were broadly classified as those of (a) primary palate or (b) secondary palate.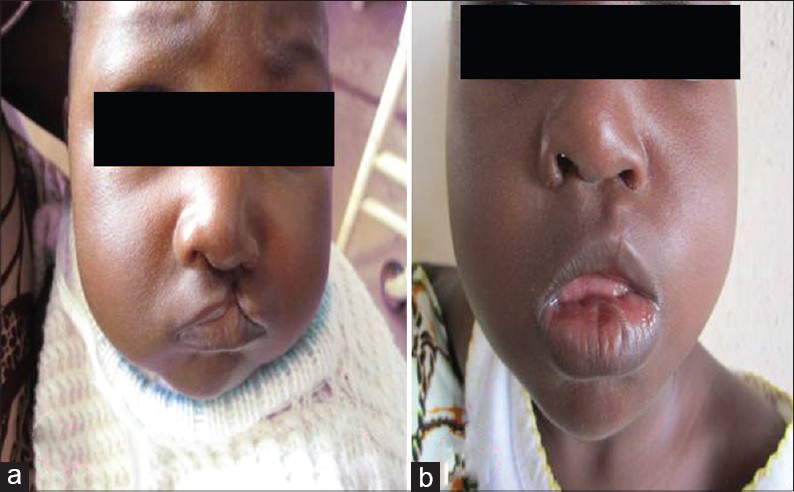 | Figure 1: Incomplete left-sided cleft of the primary palate (a) Pre-operative (b) Post-operative
Click here to view |
 | Figure 2: Complete bilateral cleft of the primary palate (a) Pre-operative (b) Post-operative
Click here to view |
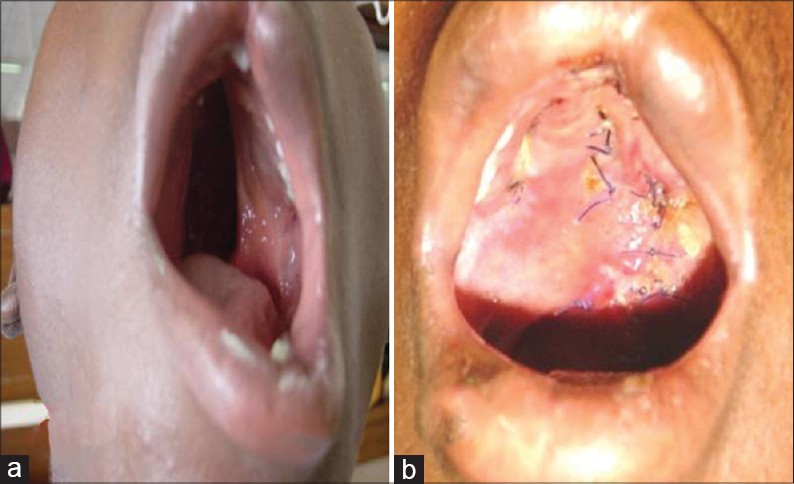 | Figure 3: Complete bilateral cleft of the secondary palate (a) Pre-operative (b) Post-operative
Click here to view |
Our surgical treatment protocol consists of early reconstruction of clefts of the primary palate with the Millard technique between the third and sixth month of age. Early closure of clefts of the secondary palate was performed with the Von Langenbeck's double palatal flap technique before the age of 2 years. However, due to delayed referrals or long surgical lists, a considerable percentage of children with clefts of the primary and secondary palate were treated after this period.
Data were analyzed for age at presentation, sex distribution, surgical technique, associated congenital anomalies and complications. The results obtained were converted to relative values in frequency tables for analysis.
| Results | |  |
The average age at presentation for all patients with cleft was 2.47 years. Patients with cleft of the primary palate presented in males at an average age of 9 months and the age of 1 year in females [Table 1]. Patients with isolated cleft of the secondary palate presented much later (mean age 4.26 years) compared to those with isolated clefts of the primary and secondary palate (mean age 2.24 years) or clefts of the primary palate (mean age 0.96 years).
Males were slightly more affected than females among all clefts with a frequency of 40 (53%) and 35 (47%). The gender distribution of clefts of the primary palate is 60% male and 20% female. Combined cleft of the primary and secondary palate showed the highest frequency 25 (33%) in males while clefts of the secondary palate were more frequent in females 10 (13%). [Table 2].
The distribution of clefts by location showed a preponderance of the left side 33 (44%), followed by right side 18 (24%) and bilateral cases 11 (15%). Male patients had the highest frequency of clefts of occurring either on the right or left sides. Bilateral clefts of the primary palate were rare constituting 4% of all clefts [Table 3].
Surgery for cleft of the primary palate was the commonest operation and constituted 32 (52%) of all the operations. The distribution of clefts according to surgical technique and timing of surgery in our center can be seen in [Table 4]. Majority of the clefts of the primary palate 24 (64%) was done after 6 months while most of the palatoplasties 28 (78%) were performed between the age of 2-4 years. Only 2 patients had cleft palate repair before the age of 1 year.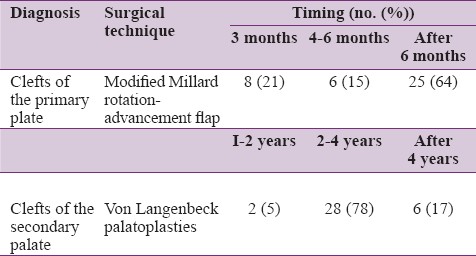 | Table 4: Distribution of clefts according to surgical technique and timing of surgery
Click here to view |
Three patients (4%) had a relative with a cleft of the primary or secondary palate. [Table 5] Male patients had a slightly higher frequency of relatives with clefts 2 (2.6%) compared to females 1 (1.3%). At least one congenital malformation coexisted with a cleft of the primary or secondary palate in 13 (17%) of the 75 babies. Of those with malformations, 7 (54%) were boys and 6 (46%) were girls. [Table 5] The commonest associated congenital anomaly was a congenital heart disease in 6 (46%) of the patients and it occurred more frequently in girls 4 (5.3%).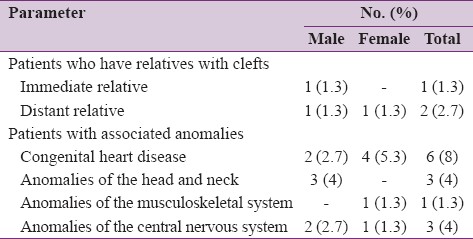 | Table 5: Distribution of patients who have relatives with clefts and associated anomalies
Click here to view |
The commonest post-operative complication of cleft of the primary palate was wound dehiscence 3 (4%). [Table 6] Fistulas 8 (10%) were the most common complication following repair of a cleft of the secondary palate. All the fistulas were symptomatic and were treated surgically. Two patients (1%) with bilateral cleft of the primary palate had flap necrosis. There was no mortality recorded during the period under review.
| Discussion | |  |
Clefts of the lip and palate are congenital anomalies that have been documented in the medical literature since the 4 th century A.D. [8] It is a problem of immense global proportion affecting in excess of 10 million people worldwide. The literature estimates the incidence of CLP (Acronym CLP; Cleft lip and palate) to be 0.8-1.6 cases for every 1000 births. [1] The estimated prevalence of cleft lip and/or palate in the Nigerian population is 0.4:1000 [12] There is a substantial phenotypic variation related to geographic origin, ethnicity, and socio-economic conditions. [9],[13] Thus, differences in presentation and morphology of clefts may occur between different cleft centers. [3]
There is a wide variation in the age at presentation in this study. Most of the patients with cleft of the primary palate presented after the age of 9 months while a higher proportion of patients with cleft of the secondary palate presented above the age of 4 years. [13] A similar finding was documented by Hodges et al.[14] in Uganda. This supports the hypothesis that patients with cleft lip and palate in developing countries tend to present at a later age due to a combination of a lack of awareness of available services and poverty. [4] Patients' awareness, access to cleft care and reliability of follow-up are established patient-related factors affecting care. In addition, difficulties with patient transportation are rampant, and often times individuals with clefts are ostracized to the most remote areas where access to transportation is poor and the ability of parents' to work and earn the money necessary for care is severely limited. [12] It is thus likely that cleft palate remains under-diagnosed in our communities and therefore is less likely to get treated promptly. Furthermore in our center and indeed many tertiary institutions in developing countries, patients with combined cleft lip and palate may not return for palatal surgery once the lip has been repaired. [15] It would be beneficial to have a more concerted effort directed toward patient, family, and societal education regarding cleft awareness, treatment options, and the importance of regular follow-up. [4],[12] It is our hope that the recent availability of charity-oriented cleft care teams would provide better access to patients with cleft lip and palate.
Worldwide, the sex distribution of clefts of the primary palate is roughly 60% male and 40% female while the distribution of clefts of the secondary palate shows a female preponderance. [13],[16] A similar pattern was found in this study. This is comparable to the study done by Habib, [17] and Blanco-Davila [18] where they found the frequency in male patients to be 61.7% and in female patients to be 38.3%. [1] A female predominance in isolated cleft palate was also noted in the Fogh Anderson study. [19] This observed pattern however contrasts with data from Caucasian populations where there is a male predominance in clefts of both primary and secondary palate. [13]
In this study, combined clefts of the primary and secondary palate, clefts of the primary palate and secondary palate were found in 62%, 21%, and 17%, respectively. [Table 2] This occurrence corresponds to many observations, including the study by McLeod et al. from Bolivia, [20] but a study by Spritz et al. in Kenya [21] showed a predominance of cleft lip compared with cleft lip and palate. [16] In contrast, most studies in Caucasian and Asian populations have reported a higher frequency of isolated cleft palate cleft of the secondary palate and clefts of both primary and secondary palate. [22],[23],[24] Although the authors attributed some of the variation to differences in study design, an analysis of comparable, small, retrospective, or hospital-based studies in low and middle income countries in Africa, Asia, and South America suggests this variation may reflect a biological phenomenon. [13] In other words, the distribution of cleft types may be determined by race and ethnicity. Alternatively, the low number of patients with isolated cleft palate in several African studies may reflect a higher mortality rate in this group associated with functional difficulties during feeding in young infants. [13]
Unilateral clefts usually predominate over bilateral clefts, and the left side is usually the most often affected. This is reflected in our study and it can be seen in [Table 3] that bilateral clefts in this study, 11 (15%) is less than the 20% that is reported in most epidemiological studies. [3] Articles that describe a link between sex and affected side are rare. One Italian study reported a link between female sex and right-sided clefts, [16] but in our study the left-sided lesion predominated in males.
Currently, there are over 170 different protocols in the management of patients with cleft lip and palate. [8],[12],[25] Most protocols are consistent in recommending early repair, typically completing primary repair of the lip and palate by the age of 2 years. [26] A commonly accepted protocol is the repair of the primary palate at 10-12 weeks of age. [8] The early timing of repair was shown to be advantageous esthetically, because the cleft is less wide at this point. Repair of the secondary palate is advocated at 9-12 months of age, before the development of speech, to maximize the development of appropriate speech patterns and to facilitate feeding. Some centers delay palatal repair until after 2 years of age, to allow for maxillary skeletal growth, and to minimize the risks of anesthesia. [8]
This study demonstrates that the average age of patients undergoing primary cleft palate repair in this center is after 6 months and repair of clefts of the secondary palate is between 2-4 years. This delay to surgery may be as a result of a number of factors. Firstly, the lack of a consistent post-natal care pathway and parent education results in delayed detection of the cleft palate particularly when the obvious cosmetic defect resulting from an associated cleft lip is not present. Additionally there remains a paucity of surgical centers capable of performing cleft surgery and, therefore, a significant financial burden is placed upon the family when travelling to these centers. [10],[12],[26] Millard's technique was the most commonly employed approach for treatment of cleft of the primary palate lip in our study. [Figure 1]b and [Figure 2]b Both the soft and hard palates were reconstructed using von Langenbeck's technique. [Figure 3]b
In this study, three patients (4%) were found to have associated family history of cleft lip and palate. Srivastavai and Bang [27] noted a family history of CLP in 11.4% of patients. Our figures may be lower because being a retrospective study, history taken may not have been exhaustive. [1] One of the most important characteristics of patients with clefts is the high incidence of associated congenital malformations compared with the incidence in the normal population. [28] The result from this study shows the frequency of associated congenital anomalies is 17.3%. Other studies have reported that this frequency can range from as low as 1.5% to as high as 63.4%. [13],[28] The wide range of reported frequencies of associated congenital anomalies have been attributed in part to the methods of data collection, with lower incidence being reported by studies that have reviewed birth certificates (not birth registries) than studies that account for patients referred to their institutions for treatment. [13],[23] Studies with higher figures are more common in live birth studies because they were dealing with newborns, whereas in this study, most patients were seen at least 3 months after birth, and therefore, most neonates could have succumbed to their anomalies. There could also have been under-reporting of associated anomalies in our study. It is also documented that some local communities neglect or even eliminate patients with congenital anomalies leading to lower prevalence of the disease. [1]
Congenital anomalies involving every organ or system may be seen in children with clefts, the incidence and site of which varies depending on the study. However, the cardiovascular system, head and neck, skeletal system, central nervous system, and the urogenital system have been reported to be the most common. [28] Cardiovascular anomalies were the most common in our series, the incidence being 6 (8%). Cardiovascular anomalies were followed by anomalies of the head and neck, central nervous system, and skeletal system.
Wound dehiscence was the commonest complication following reconstruction of the primary palate 3 (4%) in this study. Vlastos and colleagues [3] reported wound dehiscence as a complication 3.1% (2/64) following clefts of the primary palate. They also observed that immediate post-operative complications following surgical reconstruction of clefts of the secondary palate, (breathing problems and flap necrosis) was 3.6%. Fistulas 8 (10%) were the most common complication following repair of a cleft of the secondary palate in our study. All the fistulas were symptomatic and were treated surgically.
There are a few important limitations of this study. First is the nature of the study-a retrospective study. Retrospective studies are usually based on clinic records, subject to under-reporting, and may suffer from multiple sources of ascertainment bias (e.g. family history of clefts). [13] The interpretation and application of the results of this study must be considered from this standpoint. Second, the needs of patients with cleft lip and palate extend beyond surgical repair. Surgery is only a small portion of the full process. [29],[30] The importance of integrating supporting cleft care teams to successful overall outcomes cannot be overemphasized. Therefore, an integration of care with contributions of the dentists, speech-language pathologists, and audiologists is necessary to optimize outcome. Future research will be required for long-term dental evaluation, audiometric studies, and speech assessment in these patients. [13] Third, unlike many surgical conditions in which the primary goal of treatment may be the resection of a tumor or treatment of an infection that may be evaluated more directly, the goals of treating congenital conditions such as cleft lip and palate are to optimize function, aesthetic outcome, and health-related quality of life. The patients' and parents' perspective is a key component of defining outcomes in cleft lip and palate and should be included. Prospective studies are required to demonstrate measurable effects of treatment on patients from an aesthetic and health-related quality of life perspective.
| Conclusion | |  |
We found that there was a wide range of age at presentation in this study. This is characterized by late presentation for repair of clefts of the primary and secondary palate. Unilateral clefts were more common than bilateral clefts and unilateral clefts showed preponderance for the left side. Most of the other findings from our study regarding distribution of clefts of the primary and secondary palate were similar to other populations in low resource settings. We strongly support early repair of clefts to facilitate normal feeding, better speech, and ensure social acceptance.
| References | |  |
| 1. | Wanjeri JK, Wachira JM. Cleft lip and palate: A descriptive comparative, retrospective, and prospective study of patients with cleft deformities managed at 2 hospitals in Kenya. J Craniofac Surg 2009;20:1352-5. 
|
| 2. | Freeman AK, Mercer NS, Roberts LM. Nasal asymmetry in unilateral cleft lip and palate. J Plast Reconstr Aesthet Surg 2013;66:506-12. 
|
| 3. | Vlastos IM, Koudoumnakis E, Houlakis M, Nasika M, Griva M, Stylogianni E. Cleft lip and palate treatment of 530 children over a decade in a single centre. Int J Pediatr Otorhinolaryngol 2009;73:993-7. 
|
| 4. | Donkor P, Bankas DO, Agbenorku P, Plange-Rhule G, Ansah SK. Cleft lip and palate surgery in Kumasi, Ghana: 2001-2005. J Craniofac Surg 2007;18:1376-9. 
|
| 5. | Patil SB, Kale SM, Khare N, Math M, Jaiswal S, Jain A. Changing patterns in demography of cleft lip and cleft palate deformities in a developing country: The smile train effect what lies ahead? Plast Reconstr Surg 2011;127:327-32. 
|
| 6. | Adekeye EO, Lavery KM. Cleft lip and palate in Nigerian children and adults: A comparative study. Br J Oral Maxillofac Surg 1985;23:398-403. 
[PUBMED] |
| 7. | de Buys Roessingh AS, Dolci M, Zbinden-Trichet C, Bossou R, Meyrat BJ, Hohlfeld J. Success and failure for children born with facial clefts in Africa: A 15-year follow-up. World J Surg 2012;36:1963-9. 
|
| 8. | Aziz SR, Rhee ST, Redai I. Cleft surgery in rural Bangladesh: Reflections and experiences. J Oral Maxillofac Surg 2009;67:1581-8. 
|
| 9. | Pham AM, Tollefson TT. Cleft deformities in Zimbabwe, Africa: Socioeconomic factors, epidemiology, and surgical reconstruction. Arch Facial Plast Surg 2007;9:385-91. 
|
| 10. | Akinmoladun VI, Obimakinde OS, Okoje VN. Team approach to management of oro-facial cleft among African practitioners: A survey. Niger J Clin Pract 2013;16:86-90. 
[PUBMED]  |
| 11. | Kernahan DA, Stark RB. A new classification for cleft lip and cleft palate. Plast Reconstr Surg Transplant Bull 1958;22:435-41. 
[PUBMED] |
| 12. | Adetayo O, Ford R, Martin M. Africa has unique and urgent barriers to cleft care: Lessons from practitioners at the Pan-African Congress on Cleft Lip and Palate. Pan Afr Med J 2012;12:15. 
|
| 13. | Manyama M, Rolian C, Gilyoma J, Magori CC, Mjema K, Mazyala E, et al. An assessment of orofacial clefts in Tanzania. BMC Oral Health 2011;11:5. 
|
| 14. | Hodges AM, Hodges SC. A rural cleft project in Uganda. Br J Plast Surg 2000;53:7-11. 
|
| 15. | Ortiz-Monasterio F, Olmedo A, Trigos I, Yudovich M, Velazquez M, Fuente-del-Campo A. Final results from the delayed treatment of patients with clefts of the lip and palate. Scand J Plast Reconstr Surg 1974;8:109-15. 
[PUBMED] |
| 16. | Rakotoarison RA, Rakotoarivony AE, Rabesandratana N, Razafindrabe JB, Andriambololona R, Andriambololo-Nivo R, et al. Cleft lip and palate in Madagascar 1998-2007. Br J Oral Maxillofac Surg 2012;50:430-4. 
|
| 17. | Habib Z. Factors determining occurrence of cleft lip and cleft palate. Surg Gynecol Obstet 1978;146:105-10. 
[PUBMED] |
| 18. | Blanco-Davila F. Incidence of cleft lip and palate in the northeast of Mexico: A 10-year study. J Craniofac Surg 2003;14:533-7. 
[PUBMED] |
| 19. | Fogh-Andersen P. Incidence of cleft lip and palate: Constant or increasing? Plast Reconstr Surg 1962;29:720. 
|
| 20. | McLeod NM, Urioste ML, Saeed NR. Birth prevalence of cleft lip and palate in Sucre, Bolivia. Cleft Palate Craniofac J 2004;41:195-8. 
|
| 21. | Spritz RA, Arnold TD, Buonocore S, Carter D, Fingerlin T, Odero WW, et al. Distribution of orofacial clefts and frequent occurrence of an unusual cleft variant in the Rift Valley of Kenya. Cleft Palate Craniofac J 2007;44:374-7. 
|
| 22. | Calzolari E, Pierini A, Astolfi G, Bianchi F, Neville AJ, Rivieri F. Associated anomalies in multi-malformed infants with cleft lip and palate: An epidemiologic study of nearly 6 million births in 23 EUROCAT registries. Am J Med Genet A 2007;143:528-37. 
|
| 23. | Milerad J, Larson O, Hagberg C, Ideberg M. Associated malformations in infants with cleft lip and palate: A prospective, population-based study. Pediatrics 1997;100:180-6. 
|
| 24. | Cooper ME, Ratay JS, Marazita ML. Asian oral-facial cleft birth prevalence. Cleft Palate Craniofac J 2006;43:580-9. 
|
| 25. | Onah II, Opara KO, Olaitan PB, Ogbonnaya IS. Cleft lip and palate repair: The experience from two West African sub-regional centres. J Plast Reconstr Aesthet Surg 2008;61:879-82. 
|
| 26. | Butler DP, Samman N, Gollogly J. A multidisciplinary cleft palate team in the developing world: Performance and challenges. J Plast Reconstr Aesthet Surg 2011;64:1540-1. 
[PUBMED] |
| 27. | Srivastava S, Bang RL. Facial clefting in Kuwait and England: A comparative study. Br J Plast Surg 1990;43:457-62. 
|
| 28. | Altunhan H, Annagür A, Konak M, Ertuðrul S, Ors R, Koç H. The incidence of congenital anomalies associated with cleft palate/cleft lip and palate in neonates in the Konya region, Turkey. Br J Oral Maxillofac Surg 2012;50:541-4. 
|
| 29. | Raposo do Amaral CE, Cetrulo CL Jr, Pereira CL, Guidi Mde C, Raposo do Amaral CM. Augmentation gluteoplasty with dermal-fat autografting from the lower abdomen. Aesthet Surg J 2006;26:290-6. 
[PUBMED] |
| 30. | Furr MC, Larkin E, Blakeley R, Albert TW, Tsugawa L, Weber SM. Extending multidisciplinary management of cleft palate to the developing world. J Oral Maxillofac Surg 2011;69:237-41. 
|
[Figure 1], [Figure 2], [Figure 3]
[Table 1], [Table 2], [Table 3], [Table 4], [Table 5], [Table 6]
|