|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2016 | Volume
: 17
| Issue : 1 | Page : 1-4 |
|
Depression in patients with chronic low back pain: A hospital-based study
Kortor Joseph Namgwa1, Agbir Terkura2, Yongu William1, Mue D Daniel1, Elachi I Cornilius1
1 Department of Surgery, Benue State University Teaching Hospital, Makurdi, Benue State, Nigeria
2 Department of Psychiatry, Benue State University Teaching Hospital, Makurdi, Benue State, Nigeria
| Date of Web Publication | 16-May-2016 |
Correspondence Address:
Kortor Joseph Namgwa
Department of Surgery, Benue State University Teaching Hospital, Makurdi, Benue State
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/1595-1103.182478

Background: Chronic low back pain (CLBP) is a common orthopedic condition that co-exists with depression. The combination of these two contrast ailments is often associated with poorer treatment response and increase health care cost.
Objectives: To determine the prevalence of depression in patients with CLBP and study the effects of sociodemographic factors.
Materials and Methods: This is a cross-sectional study of adult patients with CLBP seen at BSUTH Makurdi from April 2014 to September 2014. Patients were assessed for depression using hospital anxiety depression scale (HADS). Data obtained were analyzed using SPSS version 16.
Results: One hundred and fourteen patients were recruited for the study, consisting of 48 males and 66 females. Age ranged from 23 to 75 years, with mean age of 44.7 years. Of 114 patients, 45 patients were found positive for depression using HADS. The rate of depression in these patients was 39.5%. The highest rate of depression was seen in 30–39 years age group.
Conclusion: The prevalence of depression in patients with CLBP was observed to be 39.5% which is comparable to the reports of previous studies in the developed countries. Keywords: Depression, low back pain, patients
How to cite this article:
Namgwa KJ, Terkura A, William Y, Daniel MD, Cornilius EI. Depression in patients with chronic low back pain: A hospital-based study. Niger J Surg Res 2016;17:1-4 |
How to cite this URL:
Namgwa KJ, Terkura A, William Y, Daniel MD, Cornilius EI. Depression in patients with chronic low back pain: A hospital-based study. Niger J Surg Res [serial online] 2016 [cited 2018 Jul 21];17:1-4. Available from: http://www.njsrjournal.org/text.asp?2016/17/1/1/182478 |
| Introduction | |  |
Depression and chronic low back pain (CLBP) are two common problems that present in health facilities. Depression is a psychiatric condition while low back pain is a physical condition which usually presents with physical symptoms.[1] The psychological and physical distress of chronic pain interacting with individual and social vulnerability may precipitate an episode of major depression.[2],[3]
Depression and pain share biological pathways and nerve transmitters with treatment implications for both conditions. Assessment and treatment of CLBP and depression simultaneously is necessary for better outcomes.[4] The explanation for this is that pessimistic thoughts activate some specific areas in the brain which cause the person to give more attention to the pain and increase the amplitude of pain felt.[4],[5]
Studies from the literature have shown depression to be highly prevalent among persons with CLBP.[6],[7],[8] Major depression is the most common mental illness associated with chronic pain. Other mental illnesses that have been described in patients with chronic pain include: Generalized anxiety disorder, posttraumatic stress disorder, and substance misuse.[9] Studies done in Nigeria have reported prevalence of CLBP of 39–59%.[10],[11],[12] Sullivan et al. and Banks and Kerns have reported the rate of major depression in patients with chronic pain of 30–54%,[5],[13] which is significantly higher than the rate of 5–8% found in general population.[14] Currie and Wang [8] also reported rates of major depression in the general Canadian population of 5.9% for pain free and 19.8% for people with chronic back pain.
Some studies in the literature have shown that either depression or CLBP may become the causative factor for the other and even exacerbate each other.[1],[15],[16] Patients suffering from depression often present with a complex set of overlapping symptoms of emotional and physical complaints like unexplained pain.[17],[18] Long standing CLBP would result into many routine changes and may adversely affect the individuals state of mind.[19],[20]
Some researchers have also studied the reverse connection, that is, patients with depression developing CLBP. One of such studies revealed that in adult males, 42% of patients who suffered primarily from depression developed CLBP, while 58% of patients had a reverse cycle of CLBP leading to depression.[21]
This is a preliminary study which was conducted to determine the prevalence of depression in patients with chronic back pain and study the effects of sociodemographic factors.
| Materials and Methods | |  |
This was a cross-sectional, descriptive, and preliminary study of patients with CLBP who were attending the orthopedic clinic of the Benue State University teaching Hospital, Makurdi, from April 2014 to September 2014. All patients who visited orthopedic clinic for the complaint of CLBP, having pain for at least 3 months and aged 20 years and above were recruited for the study. Informed consent was obtained from all the patients and this study involved only one contact with the patient for the purpose of the study. Ethical clearance was obtained from the Hospital Ethical Committee.
Patients who were severely ill and bed ridden, pregnant and lactating females and history of depression before onset of back pain were excluded from the study.
A designed questionnaire was used to obtain data. The sociodemographic data of the patient consisted of age, sex, marital status, level of education, occupation, and duration of pain.
The hospital anxiety and depression scale (HADS) was used as a screening tool for depression in this study. It is a fourteen item scale that generates ordinal data, seven of the items relate to anxiety and seven relate to depression. Each item is scored 0–3 and the total score is 21. A systematic review by Bjelland et al.[22] identified a cut-off point of 8/21 for anxiety or depression. For depression (HADS-D), the study revealed a specificity of 0.79 and a sensitivity of 0.83.
Data obtained were analyzed using Statistical Package for Social Sciences for windows, Version 16. Chicago, SPSS inc.
| Results | |  |
A total of 114 patients were recruited for the study, consisting of 48 males and 66 females with male: female ratio of 1:1.4. The mean ± standard deviation of patients' age was 44.7 ± 14.72 years (range: 23–75 years).
The age and sex distribution of patients with CLBP is shown in [Table 1]. CLBP was most frequent in the 40–49 years age group (36.0%) and least in the 70–79 years age group (0.9%).
Of 114 patients with CLBP, 45 patients were positive for depression using the HADS. The point prevalence of depression in patients with CLBP was 39.5% [Figure 1].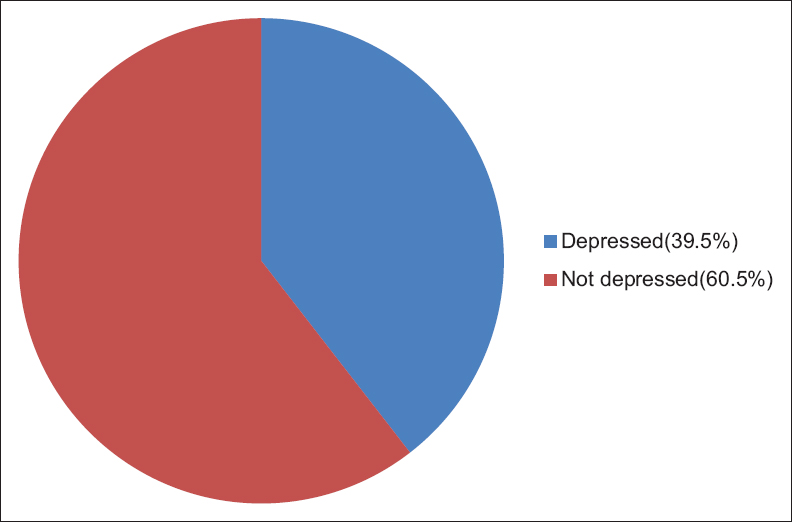 | Figure 1: Point prevalence of depression in patients with chronic low back pain
Click here to view |
[Table 2] shows the relationship between age group and depression. Among the 45 patients who were positive for depression, the highest prevalence rate was seen in 30–39 years age group (33.3%) and this was followed in the 40–49 years age group (26.7%), and the lowest was in the 70–79 years age group (2.2%). The association between age and depression was not statistically significant (P = 0.31).
Concerning gender, the prevalence was higher in the females (40.9%) than in the males (37.5%), but there was no significant association between sex and depression (P = 0.24).
As regard to the level of educational attainment, patients who have tertiary education have a prevalence of depression of 41.6%, primary education (40.6%), secondary education (40.0%), and none (31.5%) [Figure 2].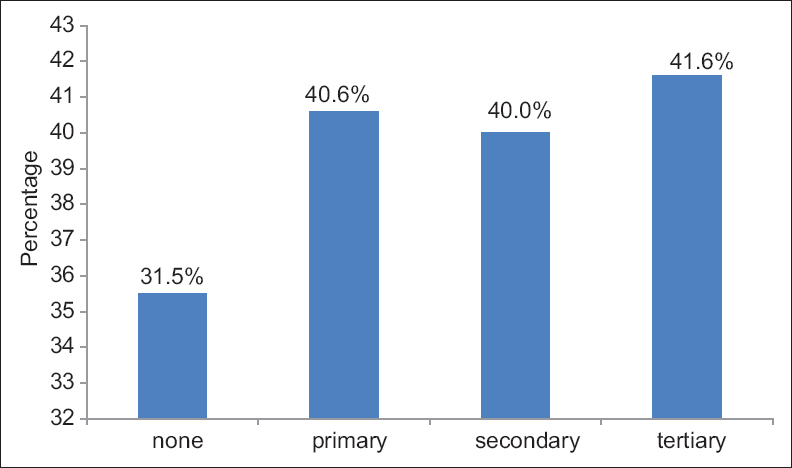 | Figure 2: Prevalence of depression in chronic low back pain by level of education
Click here to view |
Among the 45 patients with CLBP, who were positive for depression, majority of the respondents were farmers (35.6%). This was followed by civil servants (24.4%), housewives (20.0%), retirees (11.1%), and students (8.9%) [Table 3].
| Discussion | |  |
Depression is a common condition in patients with CLBP. This study found the prevalence of depression in patients with CLBP to be 39.5%. This is comparable to the rate of depression in chronic low back patients reported by Sullivan et al.[13] and Banks andKerns.[5] This rate is lower than the rate of depression, in general, population study reported by Currie and Wang.[8]
The high rate of depression in the 30–39 years and 40–49 years age groups seen in this study is consistent with the studies done by Currie and Wang [8] and Magni et al.[7] The reason for this may be attributed to the fact that this age group is the active productive age group of the society and CLBP is frequently associated with activity limitation especially farming thus the high rate of depression. There was no significant association between age and depression in patients with CLBP. Similar findings were reported by Shehab et al.[19] However, in a Canadian general population study, age was found to have significant impact on depression in patients with CLBP.[8]
The prevalence of depression in patients with CLBP in this study is higher in the females than in the males. This may be due to the fact that women have increased the risk of CLBP and higher burden for depression. This is consistent with studies done by Shehab et al.[19] and Birabi et al.[23]
Farmers have the highest rate of depression in this study. This is similar to the study done by Birabi et al.[23] This is because farming is a common occupation in Benue State and physical disability associated with CLBP would restrict farming activities. This will eventually result in poor productivity and depressive mood. There was no significant relationship of both level of educational attainment and occupation of patients with CLBP and depression.
| Conclusion | |  |
Depression is a common mental condition in patients with CLBP presenting in our health facilities. The prevalence of depression in patients with CLBP was found to be 39.5% which is comparable to the reports of previous hospital-based studies but higher than the general population studies. Age, sex, and occupation of patients did not have a significant effect on depression in patients with CLBP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Gallagher RM, Verma S. Managing pain and comorbid depression: A public health challenge. Semin Clin Neuropsychiatry 1999;4:203-20.  |
| 2. | Nicholas MK, Coulston CM, Asghari A, Malhi GS. Depressive symptoms in patients with chronic pain. Med J Aust 2009;190 7 Suppl: S66-70.  |
| 3. | Von Korff M, Simon G. The relationship between pain and depression. Br J Psychiatry 1996;168(Suppl 3):101-8.  |
| 4. | Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: A literature review. Arch Intern Med 2003;163:2433-45.  |
| 5. | Banks SM, Kerns RD. Explaining high rates of depression in chronic pain: A diathesis-stress framework. Psychol Bull 1996;119:95-110.  |
| 6. | Dworkin SF, Gitlin MJ. Clinical aspects of depression in chronic pain patients. Clin J Pain 1991;7:79-94.  |
| 7. | Magni G, Caldieron C, Rigatti-Luchini S, Merskey H. Chronic musculoskeletal pain and depressive symptoms in the general population. An analysis of the 1 st National Health and Nutrition Examination Survey data. Pain 1990;43:299-307.  |
| 8. | Currie SR, Wang J. Chronic back pain and major depression in the general Canadian population. Pain 2004;107:54-60.  |
| 9. | Demyttenaere K, Bruffaerts R, Lee S, Posada-Villa J, Kovess V, Angermeyer MC, et al. Mental disorders among persons with chronic back or neck pain: Results from the World Mental Health Surveys. Pain 2007;129:332-42.  |
| 10. | Sanya AO, Ogwumike OO. Low back pain prevalence amongst industrial workers in the private sector in Oyo State, Nigeria. Afr J Med Med Sci 2005;34:245-9.  |
| 11. | Omokhodion FO. Low back pain in a rural community in South West Nigeria. West Afr J Med 2002;21:87-90.  |
| 12. | Fabunmi AA, Aba SO, Odunaiya NA. Prevalence of low back pain among peasant farmers in a rural community in South West Nigeria. Afr J Med Med Sci 2005;34:259-62.  |
| 13. | Sullivan MJ, Reesor K, Mikail S, Fisher R. The treatment of depression in chronic low back pain: Review and recommendations. Pain 1992;50:5-13.  |
| 14. | Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003;289:3095-105.  |
| 15. | Tyrer S. Psychiatric assessment of chronic pain. Br J Psychiatry 1992;160:733-41.  |
| 16. | Atkinson JH, Slater MA, Patterson TL, Grant I, Garfin SR. Prevalence, onset, and risk of psychiatric disorders in men with chronic low back pain: A controlled study. Pain 1991;45:111-21.  |
| 17. | Katon W, Sullivan M, Walker E. Medical symptoms without identified pathology: Relationship to psychiatric disorders, childhood and adult trauma and personality traits. Ann Intern Med 2001;134:917-25.  |
| 18. | Shehab D, Al-Jarallah K, Moussa MA, Adham N. Prevalence of low back pain among physical therapists in Kuwait. Med Princ Pract 2003;12:224-30.  |
| 19. | Blier P, Abbott FV. Putative mechanisms of action of antidepressant drugs in affective and anxiety disorders and pain. J Psychiatry Neurosci 2001;26:37-43.  |
| 20. | Rush AJ, Polatin P, Gatchel RJ. Depression and chronic low back pain: Establishing priorities in treatment. Spine (Phila Pa 1976) 2000;25:2566-71.  |
| 21. | |
| 22. | Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res 2002;52:69-77.  |
| 23. | Birabi BN, Dienye PO, Ndukwu GU. Prevalence of low back pain among peasant farmers in a rural community in South South Nigeria. Rural Remote Health 2012;12:1920.  |
[Figure 1], [Figure 2]
[Table 1], [Table 2], [Table 3]
|