|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2016 | Volume
: 17
| Issue : 2 | Page : 33-37 |
|
Thromboelastography parameters versus classical coagulation profile in trauma patients: Retrospective study
Abdulraouf Y Lamoshi1, Alison M Wilson2
1 Department of Pediatric General and Thoracic Surgery, Cincinnati Children's Hospital Medical Center, Ohio, OH, USA
2 Department of Surgery, Ruby Memorial Hospital, West Virginia University, West Virginia, WV, USA
| Date of Web Publication | 16-Nov-2016 |
Correspondence Address:
Abdulraouf Y Lamoshi
2375 Montana Avenue, AP 807, Cincinnati, OH, 45211
USA
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/1595-1103.194214

Background: Thrombelastography (TEG) assesses the viscoelastic properties of the whole blood and it is more comprehensive and capable to detect any coagulation abnormalities in comparison to classical coagulation tests (CCTs). On this ground, TEG can be more efficient in acute settings. Therefore, the primary aim was to compare TEG parameters of traumatic brain injury (TBI) versus non-TBI (NTBI) patients. The secondary aim was to identify TEG versus CCT parameters associated with outcome.
Methods: A cross-sectional retrospective observational study of 142 patients admitted to a university-based, Level 1 trauma center. TEG and CCT were collected on admission. Institutional Review Board approval was obtained for this study. SAS was used for categorical data were analyzed using Chi-square or Fisher's exact test. A comparison of continuous variables between TBI and NTBI patients was performed using the independent-sample t-test.
Results: In a total of 142 patients, 48 patients had TBI and 94 patients did not. Overall, mortality was 20.4% (45.8% TBI vs. 7.4% NTBI). There were no significant associations between TEG or CCT parameters and studied variables some of which are injury severity score, abbreviated injury scale, craniotomy/ectomy, type of brain injury, discharge status, and blood pressure. There was no difference between the TBI and NTBI groups regarding TEG or CCT parameters. Maximum amplitude (MA) was the only parameter (TEG or CCT) associated with need for transfusion of packed red blood cell (PRBC) (P = 0.0377). PRBC transfusion was given in 94% of patients with an MA <57.4. Platelet transfusion was given in 89% of patients who have MA < 58.1. Fresh-frozen plasma (FFP) transfusion was given in 80% of patients who have R ≥5.8. PRBC transfusion was given in 77% of 18 patients with α <62.9.
Conclusions: TEG parameters are potentially useful as means to rapidly diagnose coagulopathy and predict transfusion in trauma patients. Independently, the presence of TBI does not cause a detectable coagulopathy. TEG analysis is more efficient than the classical parameters in detecting patients who will need PRBC and FFP transfusion. Keywords: Classical coagulation, thrombelastography, traumatic brain injury
How to cite this article:
Lamoshi AY, Wilson AM. Thromboelastography parameters versus classical coagulation profile in trauma patients: Retrospective study. Niger J Surg Res 2016;17:33-7 |
How to cite this URL:
Lamoshi AY, Wilson AM. Thromboelastography parameters versus classical coagulation profile in trauma patients: Retrospective study. Niger J Surg Res [serial online] 2016 [cited 2018 Jul 21];17:33-7. Available from: http://www.njsrjournal.org/text.asp?2016/17/2/33/194214 |
| Introduction | |  |
Blood transfusion protocols are crucial measures in all trauma settings and many other medical situations such as acute anemia due to surgical or traumatic hemorrhage, early sepsis with inadequate oxygen delivery, and acute coronary syndrome with ischemia. Choosing the appropriate timing and type of blood and/or blood product transfusions are sometimes vital decisions that determine the prognosis of trauma patients.[1] Head injury forms approximately 45% of trauma-related mortalities and bleeding is the second most common cause of death, 30% of which during the early stages of trauma.[2] On the other hand, multiorgan failure leads to 8% of deaths in the late trauma incidents, which is associated with massive transfusion.[2] In turn, massive transfusion can lead to coagulopathy in 65% of the cases (and vice versa) and increase the risk of death by 50%.[2] Thus, constructing a scientifically founded strategy to predict the precise need for transfusion to face the different scenarios can save a lot of morbidities and fatalities.[3]
Severely, injured patients may need large amounts of blood and blood products; however, there is no accurate blood tests that can predict the optimum time, type, and amount that patients really need.[4] Depending primarily on the classical coagulation laboratory tests has many limitations that may lead to deadly outcomes.[4] Posttraumatic patients, who are in hypovolemia shock, may need massive transfusion which causes the dilution of coagulation factors and platelets that in turn leads to coagulopathy disorders [5] including venous thromboembolic consequences.[6] Thrombelastography (TEG) has been used to predict the demand for specific blood products in surgeries that have high likelihood of bleeding in settings such as orthotopic surgeries, liver transplantation, cardiac surgery with the use of cardiopulmonary bypass, and in the field of trauma where it showed precise prediction for transfusion in the first day.[6] Nonetheless, TEG has not been used to measure the severity of coagulopathy based on the different types of trauma, for example, traumatic brain injury (TBI) yet.[6]
According to the previous studies, coagulopathy is more likely to develop in brain traumatic injuries patients and correlates to their high death rates.[7],[8] Although the exact correlation between TBI and disseminated intravascular coagulation (DIC) is not fully explained, as a consequence to TBI, vascular or tissue injury releases a tissue factor (thromboplastin), which stimulates other extrinsic pathway procoagulant proteins that traps platelets and activates further thrombosis including DIC.[8],[9],[10]
The primary goal of this retrospective observational study was to compare TEG parameters of TBI versus non-TBI (NTBI) patients. The secondary aim was to identify TEG versus classical coagulation test (CCT) parameters associated with the studied outcomes, which are prediction of blood and blood products transfusion need in the trauma setting.
| Methods | |  |
For TEG purposes, citrated kaolin samples were utilized. TEG machines were subjected to electronic controls three times daily and biological controls once a day (quality control). In addition to TEG and CCT values, the following variables were collected: gender, age, scene versus transferred from another hospital patients, injury severity score (ISS), abbreviated injury scale, craniotomy/ectomy, type of brain injury, discharge status (alive versus dead), blood pressure (BP), blood and blood product transfusion, hospital length of stay (LOS), and days on mechanical ventilation. The relationship between TEG and CCT parameters were analyzed using all these variables. TEG samples were sent from the trauma bay within 15 min of arrival to the hospital. TBI cases diagnosed based the on Glasgow coma scale and results of CT scan, which showed intracranial injury.
Statistical analysis was performed using SAS, version 10 (SAS Institute Inc., Cary, North Carolina, USA). Categorical data were analyzed using Chi-square or Fisher exact test. A comparison of continuous variables between TBI and NTBI patients was performed using the independent-sample t-test. Comparisons among the two groups were performed by one-way ANOVA followed by the Tukey correction for post hoc comparisons. Wilcoxon/Kruskal–Wallis tests were used when appropriate. Pearson correlation coefficients were calculated between continuous variables. P ≤ 0.05 were considered statistically significant, and data are reported as mean (standard error mean).
| Results | |  |
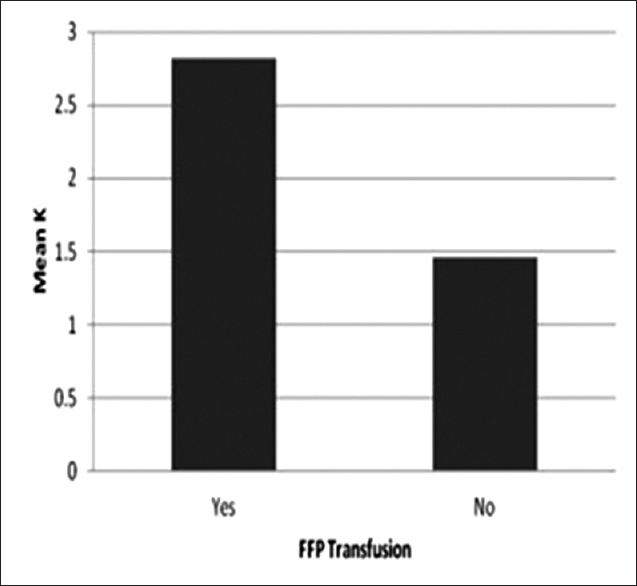
Of 142 patients, there were 44 (31%) women and 98 (69%) men. Forty-eight patients had a TBI, and 94 patients were NTBI. Overall, mortality was 20.4% (45.8% TBI vs. 7.4% NTBI). Of the 48 TBI patients, 7 (15%) were diagnosed with intraventricular hemorrhage, 22 (46%) intraparenchymal hemorrhage, 2 (4%) extradural hemorrhage, 31 (64%) subdural hemorrhage, and 26 (54%) subarachnoid hemorrhage. The patients with systolic BP (SBP) above 90 had a greater hospital LOS (6.9 days vs. 14.7 days) (P = 0.0001). In addition, SBP > 90 significantly associated with ISS where those patients who had low ISS (average of 13) had also SBP >90 and those who had high ISS (average of 19) had also SBP ≤90 (P = 003). There were no significant associations between TEG or CCT parameters and ISS, scene versus transfer, hospital LOS, or ventilator days [Table 1]. There was no difference between the TBI and NTBI groups regarding TEG or CCT parameters [Table 2]. The number of patients who was sent from the scene directly to our facility was 89 out of which 15 (17%) died during the admission. Comparably, 53 patients were transferred from other facilities out of which 14 (26%) died showing no significant difference in overall mortality (P = 0.171). This matched the severity of injuries where 38% of the scene group had ISS >15 compared with 34% of the transferred group (P = 0.611). Variables found to be associated with mortality were K (P = 0.0118) and age (P = 0.0057). [Table 1] represents the associations of all TEG and CCT parameters with the studied variables.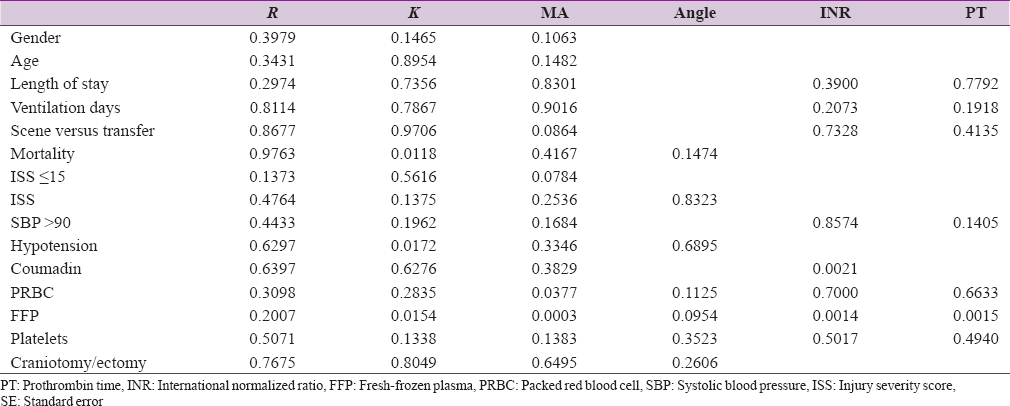 | Table 1: P value of associations of all thrombelastography and classical coagulation test parameters with the studied variables
Click here to view |
 | Table 2: Classical coagulation test and thromboelastography parameters of traumatic brain injury versus nontraumatic brain injury patients
Click here to view |
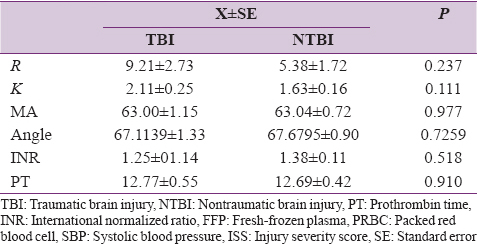
MA was the only parameter (TEG or CCT) associated with the need for transfusion of packed red blood cell (PRBC) (P = 0.0377). PRBC transfusion was given in 94% of 16 patients with MA <57.4 (1–4 units in 44% and >4 units in 50%) and only in 53% of 63 patients with MA ≥57.4 [Figure 1]. Platelet transfusion was given to 89% of 9 patients who have MA < 58.1 [Figure 2] and only in 44% of 55 patients with MA ≥58.1. In addition, fresh-frozen plasma (FFP) transfusion was given to 80% of 15 patients who have R ≥5.8 and only in 32% of 50 patients with R <5.8. Furthermore, PRBC transfusion was given in 77% of 18 patients with α<62.9 and only in 57% of 61 patients with α ≥62.9. Platelet transfusion was given to 70% of 14 patients who have α<64.5 and only in 44% of 50 patients with α ≥64.5. FFP transfusion was given to 67% of 25 patients who have α<66.3 and only in 28% of 40 patients with α ≥66.3. K value is significantly associated with mortality (P = 0.0118), hypotension (P = 0.0172), and FFP transfusion (P = 0.0154) [Figure 3].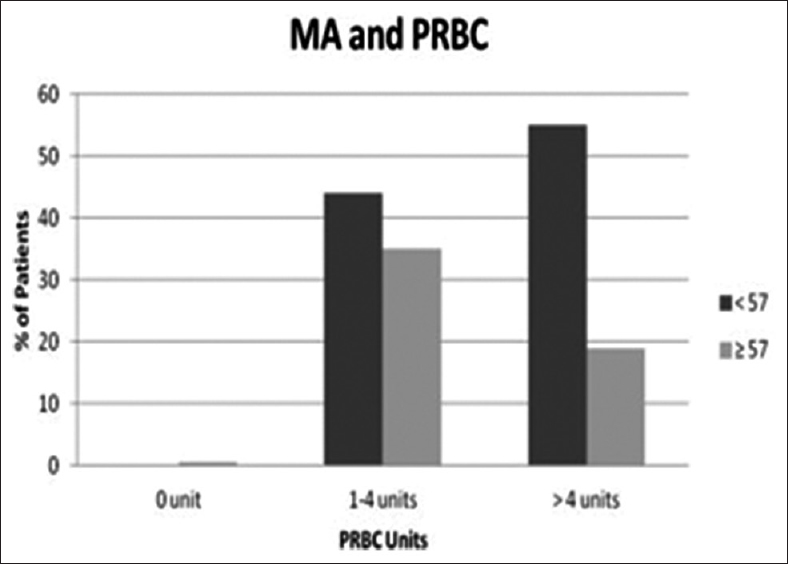 | Figure 1: Correlation of packed red blood cell transfusion with MA measurement
Click here to view |
 | Figure 3: Correlation of fresh-frozen plasma transfusion with K measurement
Click here to view |
Decreased MA (P = 0.0003), decreased K (P = 0.0154), increased PT (P = 0.0015), and increased INR (P = 0.0014) were significantly associated with FFP transfusion.
| Discussion | |  |
The main findings of this study are that when MA is less than 58.1 mm, the majority of the patients need PRBC and/or FFP. Hence, MA can represent the maximum clot strength and relates to the quality of fibrin and platelet interaction which depends on platelet number and/or function. This explains the precision and ability of MA, and the failure of CCT parameters including platelets number, to interpret such needs. Even though some changes in other parameters, K, PT, and INR, correlated with FFP transfusion that did not show a specific cutoff point nor any association with PRBC transfusion. K-time (clot formation time) represents the level of clot firmness and clot formation kinetics.
On the other hand, the CCT (INR and PT) showed only a significant association with the need for FFP transfusion, which has been also predicted by TEG parameters, MA, and K. Furthermore, CCT did not show any advantage over TEG parameters on the rest of the studied variables, including the need for blood and other blood products transfusion, hypotension, or the mortality rate. This can be explained by the limited abilities of CCT to detect the other hemostatic abnormalities that participate in their numbers are within the normal range.
We also report that there is no difference between TBI and NTBI groups regarding coagulation status that has been found by another study that stated that to develop TBI early coagulopathy, TBI patients should have a tissue injury and tissue hypoperfusion.[7],[9] In addition, our study report that low K is significantly associated with hypotension and high mortality rates (lower among those who are alive and have no hypotension). This is due to the fact that patients who are hypotensive are more prone to develop bleeding disorders and increased death rates.[9] In addition, the majority of our patients' sample did not need FFP transfusion until their R values reached 5.8. This reflects the ability of R to exclude those patients who have the least likelihood to need FFP. Furthermore, the α-angle value of <62.9 was able to predict the need of the preponderance (77%) of the sample for transfusion.
Our results are supported by the previous similar studies that showed that TEG is a valuable technique to monitor the coagulation status of TBI patients. It can differentiate between the various causes of coagulopathy and can provide appropriate guidance for blood, blood products, and other intervention.[11],[12],[13] Moreover, Maegele's study revealed that TBI patients who develop coagulopathy have about 10 times higher chance of death than those patients who do not suffer from coagulopathy.[10] In addition, Plotkin's et al. study stated that PT and PTT are unable to determine which step of the clotting flow is affected in coagulopathic patients.[11] However, employing TEG can provide a more precise diagnosis of clotting dysfunctional disorders.[11] In addition, our α-angle finding has been found by other study that showed when the parameter was utilized it predicted 84% of the patients' need for transfusion.[14]
Although blood transfusion is a vital decision that can save patients' lives, especially in emergency and operating settings, there is no a quick and trustworthy test to assess in vivo the coagulation statuses' of those patients.[11] Early transfusion of plasma and PRBC is a recommended step in the most massively bleeding and critically injured patients.[15] Nonetheless, a new study suggested that transfusing 6 platelet units for each 7–8 units of PRBC can improve the survival rates in massive transfusion patients.[15] Furthermore, giving extra cryoprecipitate units are not known to raise fibrinogen and von Willebrand's factor or carry any benefits.[15] However, TEG can provide a foundation to develop a transfusion protocol that uses patients' hemostatic statuses.[11]
This study is significant for a number of reasons. First, this study analyzed more participants (142) as compared to other studies such as Park et al.[6] (78), Plotkin et al.[11] (44), and Cohen et al.[9] (39). Second, this is the first study to our knowledge; the compares TBI with NTBI regarding TEG and CCT parameters. Third, sending the TEG samples from the trauma bay to the laboratory, within 15 min after arrival, leads to highly reliable results. This is because the samples are taken before any blood or blood products transfusion. This matches the recommended guidelines for the standard coagulation measures.[6]
However, there are a number of limitations in this study. First, it was a retrospective and a single center study. Second, some CCT results are missing. Third, transferred patients from the other facilities could spend a long time before they get TEG samples drawn and/or received blood or blood products; however, all of them came through the emergency department as a trauma activation; thus, they still have the same timeline. Fourth, fibrinogen, which is one of the most sensitive CCT, was not collected for the majority of the patients; although numerous trauma centers do not depend on this test since results are commonly not available for several hours.[14]
The major conclusion is that independently, the presence of TBI does not cause a detectable coagulopathy on admission, and MA is the best single indicator for PRBC and/or FFP transfusion in trauma patients. We also find that TEG analysis is more efficient than the classical parameters in detecting patients who will need PRBC and FFP transfusion.
Based on the current and previous work that evaluated TEG effectiveness to assess the coagulation status, this study proposes using TEG to assess the coagulation statuses of the trauma patients and predict their accurate needs for transfusions.[4],[6],[12]
We also recommend that future research should be prospective where more than one TEG test can be run on each patient, complications can be recorded, and be compared to the results of the tests (TEG or CCT) which can predict the clinical correlation. The multicentric study can eliminate any subjective bias, use the same protocol in all facilities, and avoid the above-stated limitations. In addition, we suggest further investigation of TEG's cutoff points that showed significant results in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Kaur P, Basu S, Kaur G, Kaur R. Transfusion protocol in trauma. J Emerg Trauma Shock 2011;4:103-8.  [ PUBMED]  |
| 2. | Shaz BH, Dente CJ, Harris RS, MacLeod JB, Hillyer CD. Transfusion management of trauma patients. Anesth Analg 2009;108:1760-8.  |
| 3. | Curry, Andy NG, JM Tom Pierce. Conventional and near-patient tests of coagulation. Contin Educ Anaesth Crit Care Pain 2007;7:45-50.  |
| 4. | Sankarankutty A, Nascimento B, da Luz LT, Rizoli S. TEG® and ROTEM® in trauma: Similar test but different results? World J Emerg Surg 2012;7:1-8.  |
| 5. | Johansson PI, Ostrowski SR, Secher NH. Management of major blood loss: An update. Acta Anaesthesiol Scand 2010;54:1039-49.  |
| 6. | Park MS, Martini WZ, Dubick MA, Salinas J, Butenas S, Kheirabadi BS, et al. Thromboelastography as a better indicator of postinjury hypercoagulable state than prothrombin time or activated partial thromboplastin time. J Trauma 2009;67:266-76.  |
| 7. | Talving P, Benfield R, Hadjizacharia P, Inaba K, Chan LS, Demetriades D. Coagulopathy in severe traumatic brain injury: A prospective study. J Trauma 2009;66:55-61.  |
| 8. | Stein SC, Smith DH. Coagulopathy in traumatic brain injury. Neurocrit Care 2004;1:479-88.  |
| 9. | Cohen MJ, Brohi K, Ganter MT, Manley GT, Mackersie RC, Pittet JF. Early coagulopathy after traumatic brain injury: The role of hypoperfusion and the protein C pathway. J Trauma 2007;63:1254-61.  |
| 10. | Maegele M. Coagulopathy after traumatic brain injury: Incidence, pathogenesis, and treatment options. Transfusion 2013;53 Suppl 1:28S-37S.  |
| 11. | Plotkin AJ, Wade CE, Jenkins DH, Smith KA, Noe JC, Park MS, et al. A reduction in clot formation rate and strength assessed by thrombelastography is indicative of transfusion requirements in patients with penetrating injuries. J Trauma Acute Care Surg 2008;64:S64-8.  |
| 12. | da Luz LT, Nascimento B, Rizoli S. Thrombelastography (TEG®): Practical considerations on its clinical use in trauma resuscitation. Scand J Trauma Resusc Emerg Med 2013;21:29.  |
| 13. | Chiumello D, Cressoni M, De Grandis C, Landi L, Racagni M. 24 th international symposium on intensive care and emergency medicine. Crit Care 2004;8:1-2.  |
| 14. | Jeger V, Willi S, Liu T, Yeh DD, De Moya M, Zimmermann H, et al. The Rapid TEG a-Angle may be a sensitive predictor of transfusion in moderately injured blunt trauma patients. ScientificWorldJournal 2012;2012:821794.  |
| 15. | Ketchum L, Hess JR, Hiippala S. Indications for early fresh frozen plasma, cryoprecipitate, and platelet transfusion in trauma. J Trauma Acute Care Surg 2006;60:S51-8.  |
[Figure 1], [Figure 2], [Figure 3]
[Table 1], [Table 2]
|