|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2016 | Volume
: 17
| Issue : 2 | Page : 38-42 |
|
Airway management with submental orotracheal intubation in maxillofacial surgery: Our experience and literature review
Abdurrazaq Olanrewaju Taiwo, Adebayo Aremu Ibikunle, Ramat Oyebunmi Braimah
Department of Dental and Maxillofacial Surgery, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria
| Date of Web Publication | 16-Nov-2016 |
Correspondence Address:
Adebayo Aremu Ibikunle
Department of Dental and Maxillofacial Surgery, Usmanu Danfodiyo University Teaching Hospital, PMB 12003, Sokoto
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/1595-1103.194218

Background and Aim: The challenge of the “shared airway” is a recurring predicament in maxillofacial surgeries. The need to have unfettered access to the nasal pyramid and oral cavity without jeopardizing the integrity of the airway during maxillofacial surgeries is vital. The use of submental intubation has been reported as an excellent adjunct in maxillofacial trauma surgery; however, few, if any, report exists on its use for massive facial tumors. This is a report of its use in varied scenarios including traumatic and neoplastic conditions. The aim of this study was to review the indications, complications, and outcomes of airway management using submental intubation in maxillofacial surgery at a tertiary hospital in Nigeria.
Patients and Methods: Records were retrieved retrospectively over a period of 28 months (June 2013–October 2015). Data recorded included demographics, indications, and intraoperative and postoperative complications.
Results: A total of eight patients were evaluated, all of whom had surgery under general anesthesia. All of them had conventional orotracheal intubation initially, which was then converted into the submental route. Two of them had intraoperative complications of raised airway pressure, however no postoperative complication was observed.
Conclusions: Although it requires some surgical skill, submental intubation provides a reasonable substitute to other airway management techniques in certain patients. Its importance in patients with massive maxillofacial tumors was also highlighted along with other indications. Keywords: Airway, maxillofacial, orotracheal, submental
How to cite this article:
Taiwo AO, Ibikunle AA, Braimah RO. Airway management with submental orotracheal intubation in maxillofacial surgery: Our experience and literature review. Niger J Surg Res 2016;17:38-42 |
How to cite this URL:
Taiwo AO, Ibikunle AA, Braimah RO. Airway management with submental orotracheal intubation in maxillofacial surgery: Our experience and literature review. Niger J Surg Res [serial online] 2016 [cited 2018 Jul 21];17:38-42. Available from: http://www.njsrjournal.org/text.asp?2016/17/2/38/194218 |
| Introduction | |  |
Management of the airway in maxillofacial surgeries is often challenging because of the problem of “shared airway.”[1],[2] Indeed, some craniomaxillofacial conditions, such as fractured base of the skull, nasal complex fracture, comminuted midfacial fractures, and massive maxillofacial tumors may pose the challenge of difficult airway, thus preclude the use of certain intubation techniques such as nasotracheal and conventional orotracheal intubations.[1],[3] In addition, some maxillofacial surgeries often require the use of maxillomandibular fixation, which is practically impossible to achieve while using the conventional orotracheal intubation. Moreover, alternatives such as tracheostomy or nasotracheal intubation might be contraindicated in this scenario owing to several factors.[2]
Nasotracheal intubation is not advisable in patients with fractured base of the skull, massive tumors involving both nostrils, comminuted fracture of the nasal pyramid, and septonasal deformities as this could impede effective management and inadvertent breach of the dura by the tube. The use of a nasotracheal intubation which is then switched intraoperatively to the oral route has also been postulated. It is noteworthy that this is still contraindicated in patients with fractured base of the skull.
Tracheostomy is reported to have a complication rate of 12–56%, depending on the circumstances, expertise, and available postoperative care. Its complications vary from minor to major which include scar formation, hemorrhage, tracheal stenosis, recurrent laryngeal nerve damage, trachea-esophageal fistula, and emphysema.[2] Furthermore, tracheostomy requires conscientious and attentive postoperative care.
The retromolar intubation technique which involves the passage of the endotracheal tube across the alveolar margin, between the last mandibular molar and the ascending ramus of the mandible, has also been proposed.[4] It has been touted as a simple, fast, and easy technique, which allows unconstrained access to dental occlusion intraoperatively. However, it is blighted by the unpredictability of the available retromolar space, especially in adults who have a full complement of teeth.[4] Furthermore, certain maxillofacial surgery procedures such as bilateral sagittal split osteotomy and open fixation of mandibular angle fractures may be compromised by the space taken up by the tube, which may affect access to the operative site.[5]
Submental intubation was first described by Altemir in 1986, as an alternative method of airway maintenance,[6],[7] which allows unimpeded access to the nasal pyramid and dental occlusion.[8] In this technique, the proximal end of the endotracheal tube is rerouted through the floor of the mouth and the mylohyoid muscle to exit the skin in or around the submental region.[9] Several adaptations and indications of this technique have been described.[7],[10],[11] Tracheal dissection and the risks associated with nasotracheal intubation in maxillofacial surgeries are eliminated with this technique.[12]
Prolonged use of submental intubation postoperatively is contraindicated. Therefore, patients with neurological deficit or thoracic injuries who require assisted ventilation are exempted.[9],[13] It has been used satisfactorily in different age groups with good success rates.[8],[9],[13] Overall, it is believed to have a lower morbidity than tracheostomy, requires a short period of time to perform, and has a shorter learning curve.[1] This study was to review the indications, complications, and outcomes of airway management by submental intubation in maxillofacial patients.
| Patients and Methods | |  |
The records of patients who had submental intubation for varying indications were retrieved from January 2014 to November 2015. Data recorded included demographics, indications, and intraoperative and postoperative complications [Table 1]. A total of eight patients were included.
Submental intubation technique
Orotracheal intubation of the patient was achieved initially, using an appropriately sized endotracheal tube [Figure 1]. The cuff was inflated as required and ventilation was commenced. Thereafter, routine scrubbing and draping of the patient was done. About 1.0 ml of 1:100,000 adrenaline was infiltrated subcutaneously, and a 15–20 mm skin incision was made in the submental region posterior to the central aspect of the lower border of the mandible [Figure 1]. Blunt dissection of the soft tissue layers such as subcutaneous fat, platysma, deep cervical fascia, and mylohyoid muscle was done with a curved artery forceps while maintaining contact with the lingual cortex of the mandible. A medium-sized needle holder was then passed through the incision to abut the oral mucosa, which was then incised directly over the distal end of the needle holder, and the forceps were opened to dilate the incision [Figure 2].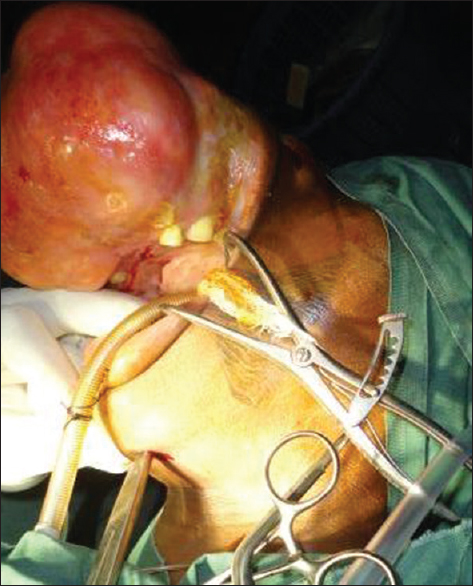 | Figure 2: A medium-sized needle holder inserted through a submental incision (note that massive maxillary tumor)
Click here to view |
The tube cuff was deflated, grasped with the needle holder, and pulled through the iatrogenic tunnel, until it was exteriorized. During the process of exteriorization, the tube was steadied by the anesthetist to avoid its unintended displacement. After successful exteriorization, the cuff was then re-inflated suitably. Subsequently, the endotracheal tube was disconnected from the ventilatory circuit and connector, after which it was also exteriorized as described earlier. Adequate suctioning of the tube end was done to rid it of any blood or debris. The connector was re-attached and the ventilatory circuit was immediately re-established. Appropriate positioning and configuration of the endotracheal tube were confirmed with the aid of auscultation, direct laryngoscopy, capnography, and airway pressure measurements. Adjustments were made to the tube position and configuration where required, and the tube was anchored by using circumferential loops of 0 silk sutures [Figure 3].
After the surgical procedure, the anchor sutures were removed, the endotracheal tube and pilot cuff were pulled through the tunnel back into the oral cavity into the conventional orotracheal intubation positioning. The cutaneous layer of the submental incision was then sutured with 3/0 nylon.
| Results | |  |
Eight patients (five females and three males) underwent submental intubation successfully, during this period of evaluation. Their age ranged from 5 years to 52 years with a mean (± standard deviation) of 11.3 (6.7). The indications for submental intubation in these cases were midfacial fractures in one case, bilateral antral cysts secondary to impacted maxillary third molar and massive obstructive maxillofacial tumors in the remaining six cases. Six cases reviewed had submental intubation done on account of massive maxillary or mandibular tumors which had profoundly impaired operative access and airway maintenance. All the submental intubations were switched back to the conventional orotracheal intubation at the end of the operative procedure, after which all the patients were extubated. The tube was retained for 13 h in one of the cases until the patient was adjudged capable of airway maintenance. The procedure was performed using nonreinforced tubes in five of the patients while the remaining three had reinforced tubes used. No postoperative complications owing to this procedure were observed in any of the patients. The oxygen saturation of all the patients was satisfactory throughout the procedure. However, two instances of raised airway pressure were noticed secondary to kinked tube, this was easily addressed by identifying the kinking and repositioning of the tube appropriately.
| Discussion | |  |
The submental intubation technique was aimed at addressing airway management challenges in oral and maxillofacial surgery. Nasotracheal intubation would have been an excellent option, but it is contraindicated in certain cases such as patients with fractured base of the skull because of the risk of passing the tube intracranially.[6] In addition, it hinders access to the nasal complex and thus makes treatment of complex midfacial fractures challenging.
Nasal intubation may also be unfeasible in patients with nasal deformities which may be acquired or congenital. Some of the cases reported had complete blockade of the nostrils and partial obliteration of the oral cavity by tumors.
Another option is retromolar intubation which often requires a semilunar ostectomy to be made in the retromolar area to allow tunneling of the endotracheal tube. It is recommended in short and uncomplicated surgeries.[6] None of our cases was suitable for this alternative.
Tracheostomy, though often used, is not without its shortfalls. It has a myriad of possible complications, ranging from the procedure-related, tube maintenance, and decannulation complications.[14] Indeed, complication rates as high as 56% for emergency tracheostomy and 12% in elective tracheostomy have been reported.[15]
However, submental intubation offers the refuge of securing the airway while having unfettered access to the nasal pyramid and the dental occlusion. Therefore, maxillomandibular fixation can be performed intraoperatively with ease and it is associated with a lower morbidity. It is easy, does not require specialized instrumentation, and less time-consuming than tracheostomy.[1],[6],[16] The submental intubation has been broadly employed in patients with fractured base of the skull, midfacial fractures, panfacial fractures, orthognathic surgery, rhinoplasty, skull-based surgery, congenital or acquired nasal deformities, and others.
However, it is contraindicated in patients who require prolonged ventilation. Modifications of the initial technique described by Altemir include avoidance of sub-periosteal dissection, use of nasal speculum, of nylon-guiding tubes, and coverage of the proximal end of the tube with a cup or glove among others. A supraperiosteal approach was utilized in all these cases, with the intraoral exit of the tube being just lateral to the lingual frenum. Although the use of reinforced tubes has been advocated because of their perceived resistance to kinking, the nonreinforced tubes were used in some of the cases seen in this series because of the resource-limited nature of our environment, though with minimal difficulty. The airway pressure and oxygen saturation were monitored closely to detect any untoward development. Raised airway pressure was noted in one patient, the cause of which was found to be the kinked tube. The tube was repositioned immediately, and the surgical procedure went on as planned. Kinking of reinforced tubes has also been reported, especially where small diameter tubes were used in children.[6] Large diameter tubes should be used where possible to reduce the likelihood of kinking.[6],[9] Kinking of endotracheal tubes is not peculiar to the submental intubation technique as it may be encountered in other techniques.[6],[12],[16]
Although proximal end of the tube was not covered with a surgical glove finger as advocated by Lima et al.,[8] there was no observed complication due to this. The proximal end of the tube was suctioned adequately before reconnection to the breathing circuit so as to eliminate any debris or fluid that may have lodged in it.
Reported complications of this technique include dislodgement of the tube, scar formation, infection, abscess, damage to the Wharton's duct, excessive hemorrhage, and damage to pilot balloon among others. All these complications may be evaded with thorough technique. Meyer et al.[17] reported abscesses and hypertrophic scar formation in 8% and 4% of the cases, respectively. None of these was noted in this report. The patients in this series had prophylactic antibiotics; 28 mg/kg of intravenous ceftriaxone 30 min to 1 h before commencement of the surgery. Interrupted suture with 3/0 nylon was also placed on the submental incision. These may have been responsible for the complete absence of infection or hypertrophic scars in this series.
The submental incision was placed centrally as described by MacInnis and Baig,[18] and the dissection was made through the soft tissues, in-between the two anterior bellies of the digastric, which is an area considered to be relatively avascular. However, the entry point of the curved artery forceps into the oral cavity was just lateral to the lingual frenum, while maintaining proximity to the lingual mandibular cortex, thus avoiding the midline structures intraorally. This was especially useful in patients with unilateral sublingual ranula as it helps in avoiding the lesion. The central location of the submental incision aids in hiding the scar if any. It is also a hair-bearing area in males which can easily camouflage any resulting scar.
In summary, many authors have reported the use of submental intubation in the management of facial fractures, but few have reported its use in the management of patients with massive maxillofacial tumors which may be complicated by blockade of the nostrils. Its use in such cases affords the surgeon with an ample access to the tumor and the dental occlusion in cases where temporary maxillomandibular fixation is needed.
In contrast, tracheostomy as an alternative to submental intubation requires meticulous maintenance and exhibits a slow learning curve. The use of fiberoptics has also been advocated; however, it requires equipment as well as training, which is a challenge in a resource-limited setting like ours. Morbidities associated with submental intubation are few when properly done.[8]
| Conclusions | |  |
Submental intubation is an important airway maintenance technique with low morbidity, and it is vital in the management of selected cases of maxillofacial trauma and massive maxillofacial tumor management where there is no need for prolonged ventilation
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Biglioli F, Mortini P, Goisis M, Bardazzi A, Boari N. Submental orotracheal intubation: An alternative to tracheotomy in transfacial cranial base surgery. Skull Base 2003;13:189-95.  |
| 2. | Thomas S, Vaithilingam Y, Sundararaman P, Thukral R, Pasupathy S. Submental intubation in maxillofacial surgery: A prospective study. J Maxillofac Oral Surg 2013;12:248-53.  |
| 3. | Malhotra N. Submento-tracheal intubation. J Anaesthesiol Clin Pharmacol 2012;28:287-90.  [ PUBMED]  |
| 4. | Prakash VJ, Chakravarthy C, Attar AH. Submental/transmylohyoid route for endotracheal intubation in maxillofacial surgical procedures: A review. J Int Oral Health 2014;6:125-8.  |
| 5. | Dutta A, Kumar V, Saha SS, Sood J, Khazanchi RK. Retromolar tracheal tube positioning for patients undergoing faciomaxillary surgery. Can J Anaesth 2005;52:341.  |
| 6. | Schütz P, Hamed HH. Submental intubation versus tracheostomy in maxillofacial trauma patients. J Oral Maxillofac Surg 2008;66:1404-9.  |
| 7. | Adeyemo WL, Ogunlewe MO, Desalu I, Akanmu ON, Ladeinde AL. Submental/transmylohyoid intubation in maxillofacial surgery: Report of two cases. Niger J Clin Pract 2011;14:98-101.  [ PUBMED]  |
| 8. | Lima SM Jr., Asprino L, Moreira RW, de Moraes M. A retrospective analysis of submental intubation in maxillofacial trauma patients. J Oral Maxillofac Surg 2011;69:2001-5.  |
| 9. | Caubi AF, Vasconcelos BC, Vasconcellos RJ, de Morais HH, Rocha NS. Submental intubation in oral maxillofacial surgery: Review of the literature and analysis of 13 cases. Med Oral Patol Oral Cir Bucal 2008;13:E197-200.  |
| 10. | Green JD, Moore UJ. A modification of sub-mental intubation. Br J Anaesth 1996;77:789-91.  |
| 11. | Saheb SM, Nath VN, Kumar KP, Padmaja PP. A novel method using Seldinger's technique for submental intubation in major craniomaxillofacial fractures: A case series. Indian J Anaesth 2014;58:48-50.  [ PUBMED]  |
| 12. | Yadav SK, Deo G. Submental intubation including extubation: Airway complications of maxillomandibular fixation. Case Rep Anesthesiol 2012;2012:841051.  |
| 13. | Caron G, Paquin R, Lessard MR, Trépanier CA, Landry PE. Submental endotracheal intubation: An alternative to tracheotomy in patients with midfacial and panfacial fractures. J Trauma 2000;48:235-40.  |
| 14. | Cipriano A, Mao ML, Hon HH, Vazquez D, Stawicki SP, Sharpe RP, et al. An overview of complications associated with open and percutaneous tracheostomy procedures. Int J Crit Illn Inj Sci 2015;5:179-88.  [ PUBMED]  |
| 15. | Hamid AA, Sattar F, Din SE, Khan NS, Ullah Z. Complications of tracheostomy. J Postgrad Med Inst (Peshawar Pak) 2011;18:3.  |
| 16. | Khan I, Sybil D, Singh A, Aggarwal T, Khan R. Airway management using transmylohyoid oroendotracheal (submental) intubation in maxillofacial trauma. Natl J Maxillofac Surg 2014;5:138-41.  [ PUBMED]  |
| 17. | Meyer C, Valfrey J, Kjartansdottir T, Wilk A, Barrière P. Indication for and technical refinements of submental intubation in oral and maxillofacial surgery. J Craniomaxillofac Surg 2003;31:383-8.  |
| 18. | MacInnis E, Baig M. A modified submental approach for oral endotracheal intubation. Int J Oral Maxillofac Surg 1999;28:344-6.  |
[Figure 1], [Figure 2], [Figure 3]
[Table 1]
|