|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2016 | Volume
: 17
| Issue : 2 | Page : 48-52 |
|
Improvisation of surgical equipment in the surgical services of a developing country
Adeyinka Ayodele Adejumo1, Oluseyi A Adeosun1, Paul O Omoregie1, Barnabas Alayande2
1 Department of Surgery, Federal Medical Centre, Keffi, Nigeria
2 Department of Surgery, Jos University Teaching Hospital, Jos, Nigeria
| Date of Web Publication | 16-Nov-2016 |
Correspondence Address:
Adeyinka Ayodele Adejumo
P.O. Box 324, Gwagwalada, FCT Abuja
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/1595-1103.194217

Background: The perennial scarcity of surgical equipment in Nigeria has given room for improvisation of such items using locally available materials.
Aim: This publication aims to appraise the ingenious methods employed by surgeons to overcome their challenges in clinical practice.
Methods: An in-depth research into relevant literature about the functionality of various surgical devices was carried out using selected texts and relevant articles.
Results: Many surgeons have come up with various techniques to make do with local resources in overcoming the limitations imposed by scarcity of certain equipment/device.
Conclusion: Surgical practitioners in resource-limited regions have been able to surmount the challenges of scarcity of required items using different methods and materials from the local environment. Keywords: Improvisation, limited resources, surgery practice
How to cite this article:
Adejumo AA, Adeosun OA, Omoregie PO, Alayande B. Improvisation of surgical equipment in the surgical services of a developing country. Niger J Surg Res 2016;17:48-52 |
How to cite this URL:
Adejumo AA, Adeosun OA, Omoregie PO, Alayande B. Improvisation of surgical equipment in the surgical services of a developing country. Niger J Surg Res [serial online] 2016 [cited 2018 Jul 21];17:48-52. Available from: http://www.njsrjournal.org/text.asp?2016/17/2/48/194217 |
| Introduction | |  |
Surgical practice in Nigeria and the sub-Saharan Africa is confronted with many challenges. These challenges are encountered in the process of caring for our patients either before, during, or after a surgical procedure is embarked upon. Many times, these challenges could pose a barrier to achieving the desired goal of treatment. This is due to various but interwoven factors that have crippled the growth of all arms of the economy as a whole.[1],[2]
Surgical practice in Nigeria cut across both urban and rural areas with a majority of the patients dwelling in the rural areas not having access to proper health-care centers and specialists care. Moreover, most hospitals in the urban areas are also plagued with lack required equipment needed to work optimally.[2],[3] In order to surmount these challenges, many surgeons and practitioners have devised ways to make do with locally available materials to modify and/or construct devices that will make their practice worthwhile and achieve the desired result which can be compared with that of their contemporaries in the developed settings.
| Why the Need for Improvisation? | |  |
Improvisation is critical to surgical practice, especially in the sub-Saharan Africa. The reasons for this are undoubtedly clear. The teeming populace with attendant poor health-care facilities has made it paramount to look at alternative sources of getting required hospital/surgical items from the local environment. This does not only make the cost of surgery cheaper and affordable for the patients but also gives satisfaction to the surgeon. Generally speaking, we may consider the need for improvisation as being patient-related, supply-related, or a combination of the two factors.
Patient-related factors have to do with the financial power of the patient and his/her relations. Most of the times, the patients pay out of pocket to get medical treatment and also get other hospital consumables. This invariably make patients seek for alternative methods of treatment from quacks. The nonavailability of some equipment/items could pose as bottlenecks along the line of management of patients. These may either delay the surgery thereby prolonging the disease or even alter the line of management postoperatively. Most of the times, these are the reasons for undeserved morbidity and mortality in our setting.
On the other hand, the scarcity of some of the items may not be unrelated to lack of availability in our hospitals. The time taken for the supply of such items while following the “due process” may be unduly prolonged. Moreover, some of the suppliers choose what to supply and not what is needed. At the end, there is a scarcity of one thing or the other. These independent but interwoven factors are reasons why there is a scarcity of some expected equipment in many of our hospitals.
| Attributes of Improvised Devices | |  |
Pivotal factors that must be considered when improvising any item should bear into cognizance the fact that such item should be cost effective, locally and readily available, biomechanically efficient, and technologically simple. Improvisation must conform to the underlying principles of function it intends to subserve. These are paramount and nonnegotiable factors that must always be considered when improvising for any medical device. Obviating the underlying scientific principle of any device automatically overrules the need for its improvisation to overcome a complex technology.
| Types of Improvisation | |  |
Surgical practice in Nigeria has survived the scarcity and nonavailability of some equipment over the decades. There is no surgical subspecialty that is exempt from the various ingenious methods that have been designed by our surgeons in order to overcome their challenges. Some of the various types of improvisation are discussed below.
Improvised thoracostomy tube
The underwater-sealed thoracostomy tube works basically on the principle of pressure difference between the pleural cavity and the atmosphere. This principle is reproduced and maintained while constructing a chest tube using a 1.5 L plastic bottled table water container connected to the chest tube [4],[5] (at times, the chest tube itself is improvised using size 24G Foley catheter or Nelaton's catheter). The system remains underwater sealed, and it is able to drain the pleural cavity as efficient as the standard apparatus [Figure 1].[6] Surgeons that use the Foley catheter for improvised chest tube have complained that it kinks easily and causes some obstruction to the egress of effluent. Superficial surgical site infections, as well as residual hemothorax, are complications that have been observed by the users.[7]
Feeding gastrostomy
This is a procedure that is often performed in cases of esophageal or laryngeal pathologies in order to feed the patient. The standard gastrostomy tube is not readily available; hence, the use of a wide caliber (size 24 Fr) Foley catheter with a spigot. Blended food and liquids are usually introduced through the open end using a large caliber syringe under gravity [Figure 2]. This method is widely employed by many surgeons who have found it quite useful for adequate nutritional rehabilitation of many patients with esophageal lesions with little or no complications reported.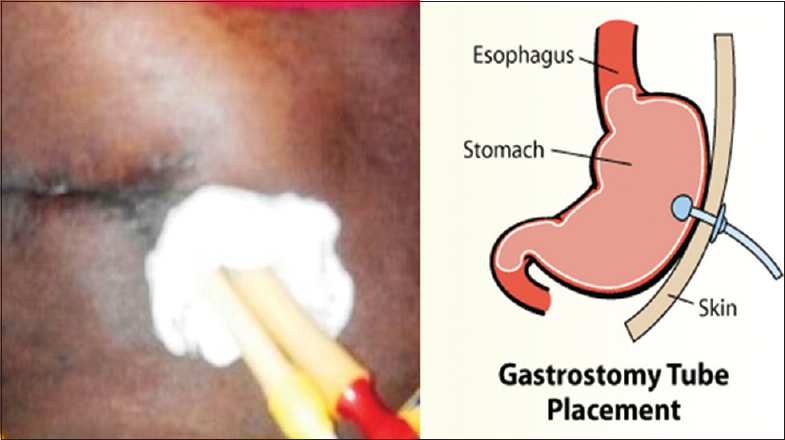 | Figure 2: Improvised gastrostomy tube (adjacent picture showing the mechanism of gastrostomy tube)
Click here to view |
Tourniquet
This is invaluable equipment, especially to the orthopedic surgeons when a bloodless operative field is desired. The availability of the electrically inflatable type in most of our hospitals is a far cry. In addition, the nonavailability of appropriate cuff for different age groups and body built is a confounding factor. In order to bridge this gap, an improvised device that will obviate the above-mentioned challenges has been designed using the inner tube of the bicycle tyre. This is made into different sizes with variations in length and width; readily available and can be easily managed at all tiers of health-care delivery. Though simple as it may be, all precautions as to the use of tourniquet must be strictly followed. The application of improvised tourniquet is usually at the discretion of the surgeon as there is no objective way of estimating the pressure being applied; this is a major limitation to the use of this device. This becomes important with regard to tourniquet palsy that may ensue; however, this is not usually encountered as the tourniquet is adequately padded and tourniquet time is strictly followed. Reperfusion injury is a life-threatening complication that may ensue following prolonged application of tourniquet; hence, the surgeon is responsible for the application and removal of the tourniquet as at when due and this responsibility should not be delegated to any other person.
Drains
The use of drains in surgical practice remains invaluable component of surgery.[8] To the general surgeon, this may be employed to aid the egress of effluent from a septic abdomen, thyroidectomy, mastectomy, and common bile duct drainage after exploration. The orthopedic surgeons also make use of the drain after performing an amputation or open reduction and internal fixation or arthroplasty to prevent hematoma collection.[9] Plastic surgeons also make use of drain after raising a flap to prevent seroma or hematoma collection which may preclude the survival of such flap.[10]
More often than not, surgeons will prefer a closed active drain in order to keep the patient clean, prevent the retrograde ascent of infection and enables quantification of effluent.[10] However, most hospitals in Nigeria do not have the luxury of this equipment. This challenge is overcome by the use of a wide caliber syringe connected to a feeding tube and this creates a negative suction pressure required.[10] An alternative to this is using fenestrated Foley catheters or a nasogastric tube [Figure 3]. These improvised drains are in turn connected to a urine bag or an unpunctured intravenous fluid bag to receive the effluent. This creates a closed system that closely follows the principle on which active drain works. Blockade of the tube (as a result of kinking or patient lying on the tube) has been observed by many practitioners to be a limiting factor. The use of nasogastric tube is often confronted with dislodgement as the expected tissue reaction required to initiate fibrosis is usually absent. Hence, proper anchorage is paramount.[11]
Silo
The use of silo in the management of omphalocele or gastroschisis is inestimable. This device is employed to prevent fluid evaporation from the bowels as well as assist in the gradual return of the eviscerated bowel back into the abdominal cavity.[12],[13] The urine bag is usually used to achieve this aim. The urine bag is sutured to the deep fascia around the edge of the defect and twisted on a daily basis to achieve gradual bowel reduction [Figure 4]. Other items that can be improvised for a silo include softened infusion bags or prewashed sterile female condom (without spermicide).[14] This and many more improvisations have been made by pediatric surgeons in order to get the work done in resource-limited environment like ours.[15] The limitations to the use of silos by practitioners in this environment are the nonavailability of neonatal ventilators that is needed to augment the cardiorespiratory activities of the patient as a result of respiratory comprise that could ensue from bowel reduction, especially in patients with large abdominal defects. Reported complications that have observed with the use of silos include respiratory tract infection and death (due to compartment syndrome).[12] These were largely seen in patients with large defects in whom ventilator support could not be achieved.
Ventriculoperitoneal shunt
The use of shunt in the management of hydrocephalus cannot be underestimated. Neurosurgeons practicing in this region have devised a means of overcoming the perennial problems of scarcity of a standard external ventricular drain with a feeding tube [Figure 5]. This has led to a significant reduction in the mortality associated with hydrocephalus patients who could not get timely intervention due to scarcity of the customized shunt.[16] The limitation to the use of the feeding tube is the fact that it cannot stay for longer periods, unlike the antibiotic-impregnated tubes that could stay for as long as 10 days or more. Infection has been documented to be the most common complication observed with the use of feeding tube as a ventriculoperitoneal shunt.[16]
| Lessons Learned | |  |
Practicing surgery in the third world countries could be challenging and limiting. However, it has come to the limelight that we can still practice effectively and efficiently with the limited resources within our reach. Although we may not have all the luxury and paraphernalia expected of a world class health system, but we can still boast of having good management outcome that is comparable to centers in the developed setting. To this end, surgeons practicing in the developing world should be applauded with the level of ingenuity they have devised to overcome their challenges.
| The Future | |  |
As a country and the most populous nation on the continent, we should endeavor to see how we can make surgical/hospital consumables readily available and affordable using locally available materials which could be designed to suit our needs. This could entail collaborative efforts with our higher institutions of learning to see how we can revolutionize out health-care industry with indigenous technology and raw materials. Interagency collaboration will also harness the raw materials needed from the various sectors such as petrochemical products, iron and steel, solid minerals, and energy with less dependence on imported products.[17] These cohesive efforts will of course reduce the amount of foreign exchange spent on imported consumables, provide job opportunities for our graduates, and put the nation at the front burner in terms of technological revolution in Africa.
| Conclusion | |  |
It is obvious that surgical practice in a resource-limited environment like ours is confronted with myriads of constraints. These limitations should serve as a pedestal that will make us to look inward with a vision of being a self-sustaining nation that can meet her needs by tapping into both human and natural resources being underutilized at present.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Duru EJ, Nwagbos CI. The problems and prospects of public health care development in Nigeria's local government system. Glob J Soc Sci 2007;6:51-6.  |
| 2. | Uneke C, Ogbonna A, Ezeoha A, Oyibo P, Onwe F, Ngwu B. The Nigeria health sector and human resource challenges. Internet J Health 2007;8:1-5.  |
| 3. | Federal Ministry of Health (FMOH). Health Systems Development Project II. Abuja: Federal Ministry of Health; 2000.  |
| 4. | Ogirima MO. An improvised active drain. Niger J Surg Res 2000;2:161-3.  |
| 5. | Edaigbini SA, Delia IZ, Aminu MB, Orogade AA, Anumenechi N, Aliyu ID. Indications and complications of tube thoracostomy with improvised underwater seal bottles. Niger J Surg 2014;20:79-82.  [ PUBMED]  |
| 6. | Aduful HK, Adu-Aryee NA, Anyawu CH, Archampong EQ, Yeboah ED, Dakorak TK. Management of the injured patients: Penetrating and non-penetrating injuries. In: Badoe EA, Archampong EQ, da Rocha-Afodu JT, editors. Principles and Practice of Surgery Including Pathology in the Tropics. 4 th ed. Accra: Ghana Publishing Corporation; 2009. p. 165-70.  |
| 7. | Iribhogbe PE, Uwuigbe O. Complications of tube thoracostomy using advanced trauma life support technique in chest trauma. West Afr J Med 2011;30:369-72.  |
| 8. | Makama JG, Ameh EA. Surgical drains: What the resident needs to know. Niger J Med 2008;17:244-50.  |
| 9. | Parker MJ, Roberts C. Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev 2001;4:CD001825.  |
| 10. | Esezobor EE, Okumayin AA. The syringe suction drain-a unique improvisation in rural plastic surgery practice. Niger J Plast Surg 2012;8:70-3.  |
| 11. | Irabor DO, Oyegbile IO, Ladipo JK, Adegoke PA. Where there is no T-tube: Operative management of 2 patients with cholelithiasis. Niger J Surg Res 2002;4:57-61.  |
| 12. | Uba AF, Chirdan LB. Omphalocoele and gastroschisis: Management in a developing country. Niger J Surg Res 2003;5:57-61.  |
| 13. | Osifo OD, Ovueni ME. The prevalence, patterns, and causes of deaths of surgical neonates at two African referral paediatric surgical centres. Ann Pediatr Surg 2009;5:194-9.  |
| 14. | Bustorff-Silva JM, Schmidt AF, Gonçalves A, Marba S, Sbragia L. The female condom as a temporary silo: A simple and inexpensive tool in the initial management of the newborn with gastroschisis. J Matern Fetal Neonatal Med 2008;21:648-51.  |
| 15. | Meier D. Opportunities and improvisations: A pediatric surgeon's suggestions for successful short-term surgical volunteer work in resource-poor areas. World J Surg 2010;34:941-6.  |
| 16. | Ojo OA, Asha MA, Bankole OB, Kanu OO. Improvised external ventricular drain in neurosurgery: A Nigerian tertiary hospital experience. J Neurosci Rural Pract 2015;6:304-8.  [ PUBMED]  |
| 17. | Oyemakinde A, Nguku P, Babirye R, Gitta S, Nsubuga P, Nyager J, et al. Building a public health workforce in Nigeria through experiential training. Pan Afr Med J 2014;18 Suppl 1:1.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
|