|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2015 | Volume
: 10
| Issue : 3 | Page : 87-90 |
|
Study of bone markers in hyperthyroidism: Single center experience from South India
Babulreddy Hanmayyagari1, Mounika Guntaka2, Rakesh Sahay3, Jayanthy Ramesh3, Sri Nagesh4
1 Department of Endocrinology, Krishna Institute of Medical Sciences, Chalmeda Anand Rao Institute of Medical Sciences, Karimnagar, Telangana, India
2 Department of Biochemistry, Chalmeda Anand Rao Institute of Medical Sciences, Karimnagar, Telangana, India
3 Department of Endocrinology, Osmania General Hospital, Chalmeda Anand Rao Institute of Medical Sciences, Karimnagar, Telangana, India
4 Department of Endocrinology, Care Hospital, Hyderabad, Chalmeda Anand Rao Institute of Medical Sciences, Karimnagar, Telangana, India
| Date of Web Publication | 21-Oct-2015 |
Correspondence Address:
Babulreddy Hanmayyagari
Flat No. A 904, Sri Sai Ram Towers, Beside Alwyn Colony Water Tank, Hafeezpet, Hyderabad - 500 049, Telangana
India
  | Check |
DOI: 10.4103/1858-5000.167867 
Aim: To evaluate bone health markers and Vitamin D status in patients with hyperthyroidism comprehensively, and comparison of same with matched controls. Materials and Methods: The study has been done on 30 newly diagnosed hyperthyroid patients and matched controls. Cases were selected after careful exclusion of conditions which adversely affect bone health. Statistical comparisons were performed with Student's t-test. Results: The study group has shown normal calcium (20% had hypocalcemia), normal phosphorus, normal parathyroid hormone values, raised alkaline phosphatase levels, and significant rise in both bone formation (osteocalcin) and resorption (β-cross laps) markers (P < 0.05). In addition, 95% of our subjects (patients and controls) were Vitamin D deficient (mean - 17.2 ng/dl). Conclusion: Hyperthyroidism is associated with increased rate of bone remodeling and changes in mineral homeostasis, thereby increases fracture risk. Associated Vitamin D deficiency further deteriorates bone quality. Hence, we suggest therapeutic Vitamin D and calcium supplementation is needed in addition to antithyroid medication. Keywords: β-crosslaps, hyperthyroidism, osteocalcin, Vitamin D
How to cite this article:
Hanmayyagari B, Guntaka M, Sahay R, Ramesh J, Nagesh S. Study of bone markers in hyperthyroidism: Single center experience from South India. Sudan Med Monit 2015;10:87-90 |
| Introduction | |  |
Hyperthyroidism is a common endocrine disorder associated with the significant impact on bone health. Predominant effects seen are increased rate of bone remodeling thereby changes in mineral homeostasis ultimately leading to a reduction in bone mineral density (BMD). These changes in turn associated with osteoporosis, so increased fracture risk. [1]
However, the changes in BMD occur only slowly, making it difficult to judge the benefits, if any, of antithyroid medication. Early identification of those individuals at risk of long-term reduction in BMD caused by thyrotoxicosis may enable early therapeutic intervention. A number of biochemical markers reflects the rapid bone turnover in thyrotoxicosis early in the disease course and their role in the prediction of BMD established recently. [2]
There is a scarcity of data on bone markers in thyrotoxicosis from India. Western data suggest that these patients have hypercalcemia, hyperphosphatemia, raised alkaline phosphatase, and suppressed parathyroid hormone (PTH). Available small data from Northern India suggests that due to concomitant Vitamin D deficiency these patients have normal calcium levels and increased bone loss, but the authors not performed bone markers in their study. Recently, a study also showed a high prevalence of Vitamin D deficiency in South Indian population. [3] Hence, we have chosen this topic to study Vitamin D status, bone health markers and the effect of Vitamin D deficiency on bone health in our thyrotoxic patients.
| Materials and methods | |  |
The study has been done on a group of hyperthyroidism and matched controls, attending to our center, during the period of May to December 2008. Both inpatients and outpatients were included. Totally, 100 cases of hyperthyroid patients were screened and 30 cases were selected for the study (five male patients were screened but excluded because all of them were smokers), control group consisting of 20 subjects who were matched by the hyperthyroid group as far as possible. Total calcium and Vitamin D intake/day calculated in all subjects by a dietary recall method with the help of a dietician.
Inclusion criteria
The subjects of 18-45 years who are having fairly regular cycles with symptoms and signs of thyrotoxicosis for at least 3 months and who were not used the antithyroid medication in the past.
Exclusion criteria
Parity > 3 children, postmenopausal, amenorrhea >6 months (include pregnancy, lactation), smokers, drugs, which interfere with bone turnover (betablockers, diuretics, oral contraceptive pills, calcium supplements, etc.), H/O malabsorption (pancreatitis, bowel surgery). In view of all these factors can interfere adversely with bone turnover.
Statistical analysis
Parameters are expressed as mean ± 1 standard error of the mean, statistical comparisons were performed with Student's t-test. Calculations were performed using SPSS software (version 10.0) IBM corporation, a P ≤ 0.05 was considered statistically significant.
Biochemical measurements
Serum samples were collected from all patients before 9 a.m. after an overnight fast. The samples were immediately processed and kept frozen at −70°C until the assays were performed. Serum calcium and serum phosphorus were determined by spectrophotometric analysis, alkaline phosphate measured by the p-nitrophenylphosphate kinetic method. Serum 25(OH)D was measured by radioimmunoassay, and intact PTH was determined by chemiluminescence assay (cold chain maintained from syringe to storage).
Osteocalcin measured by the highly specific immunoenzymometric assay (kits provided by biosource Europe S.A Rue de l'Industrie 8, B-100 Nivelles, Belgium). β-crosslaps were measured by electro-chemiluminescence.
| Discussion | |  |
In this study, all of our patients had newly diagnosed hyperthyroidism, presumably of several months of duration and is associated with observable changes in bone mineral metabolism and bone markers [Table 1] and [Table 2].
The majority of patients with hyperthyroidism in the west had normal or increased serum total calcium levels, hyperphosphatemia, and suppressed PTH levels than controls. [4] All of the above effects are due to increased bone resorption in thyrotoxicosis due to the direct effect of T 3 on the bone. [5] Our patients with thyrotoxicosis are different from the western patients from the bone mineral homeostasis point of view. These patients have normal calcium (in fact 20% had hypocalcemia), normal phosphate, and PTH levels, this is due to of associated subclinical Vitamin D deficiency in our group, recent data confirmed that there is widespread Vitamin D deficiency in South Indian population. [3] This can further deteriorate bone quality in this population. These bone mineral parameters were well correlated with available Indian data. [6]
Hyperthyroidism is characterized by increased bone turnover and bone resorptive activity. [7] We observed this in our study where both bone formation and resorption parameters were elevated [Figure 1] and [Figure 2]. In the hyperthyroid status the initiation rate of new remodeling cycles is significantly increased. However, the total work performed by resorptive cells (i.e., the final resorption depth) is unchanged, whereas the total work performed by osteoblasts (i.e., the mean thickness of completed walls) is reduced. The normal cycle duration of approximately 200 days is halved in thyrotoxicosis. Thus, during the thyrotoxic status resorption markers increase much more than formation markers (the same was observed in our study). This reflects unbalanced bone turnover in favor of bone resorption and is probably due to some degree of direct inhibition of osteoblasts by high thyroid hormone levels. A reversal above pattern seen with treatment of hyperthyroidism [8] (increase in formation markers than resorption markers).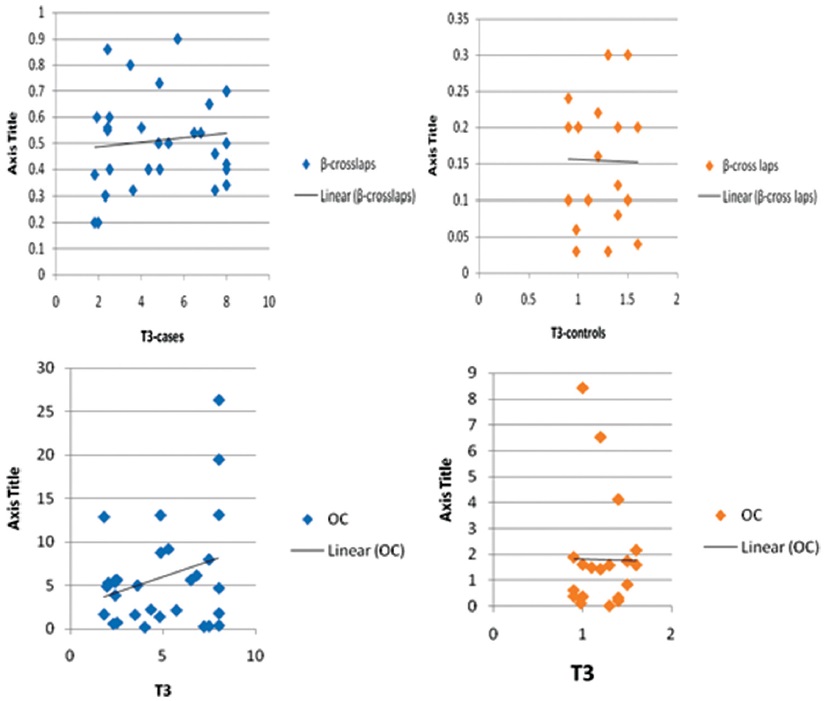 | Figure 1: Comparison of correlations between serum osteocalcin, T3, and â-crosslaps, T3 in cases and controls
Click here to view |
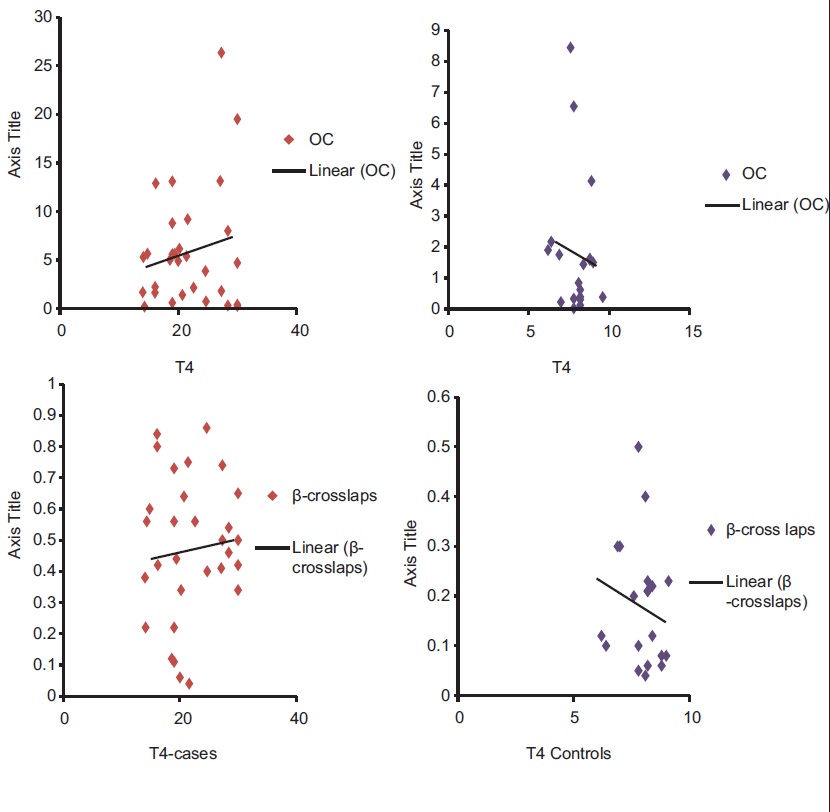 | Figure 2: Comparison of correlations between serum osteocalcin, T4, and â-crosslaps, T4 in cases and controls
Click here to view |
| Conclusions | |  |
Hyperthyroidism is associated with increased rate of bone remodeling and changes in mineral homeostasis, thereby increases fracture risk. Associated Vitamin D deficiency in hyperthyroid patients further increases bone turnover thereby adversely affects bone quality. Therefore, therapeutic doses of Vitamin D and calcium supplementation to correct Vitamin D deficiency and continuous calcium supplementation in addition to antithyroid medication will improve bone quality in hyperthyroid patients and further larger studies are needed on this issue.
Limitations of the study
The sample size is small, so large-scale studies are needed to confirm these findings. The status of bone mineral metabolism and bone markers was not studied after euthyroidism is achieved. As all of our patients (cases and controls) are Vitamin D deficient, bone health markers in Vitamin D sufficient group needs to be done.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Fraser SA, Anderson JB, Smith DA, Wilson GM. Osteoporosis and fractures following thyrotoxicosis. Lancet 1971;1:981-3.  |
| 2. | Hari Kumar KV, Muthukrishnan J, Verma A, Modi KD. Correlation between bone markers and bone mineral density in postmenopausal women with osteoporosis. Endocr Pract 2008;14:1102-7.  |
| 3. | Harinarayan CV, Ramalakshmi T, Prasad UV, Sudhakar D, Srinivasarao PV, Sarma KV, et al. High prevalence of low dietary calcium, high phytate consumption, and vitamin D deficiency in healthy south Indians. Am J Clin Nutr 2007;85:1062-7.  |
| 4. | Mosekilde L, Eriksen EF, Charles P. Effects of thyroid hormones on bone and mineral metabolism. Endocrinol Metab Clin North Am 1990;19:35-63.  |
| 5. | Manicourt D, Demeester-Mirkine N, Brauman H, Corvilain J. Disturbed mineral metabolism in hyperthyroidism: Good correlation with tri-iodothyronine. Clin Endocrinol (Oxf) 1979;10:407-12.  |
| 6. | Dhanwal DK. Bone mineral metabolism in thyrotoxicosis. Indian J Endocrinol Metab 2007;11:33-6.  |
| 7. | Siddiqi A, Burrin JM, Noonan K, James I, Wood DF, Price CP, et al. A longitudinal study of markers of bone turnover in Graves' disease and their value in predicting bone mineral density. J Clin Endocrinol Metab 1997;82:753-9.  |
| 8. | Garnero P, Vassy V, Bertholin A, Riou JP, Delmas PD. Markers of bone turnover in hyperthyroidism and the effects of treatment. J Clin Endocrinol Metab 1994;78:955-9.  |
[Figure 1], [Figure 2]
[Table 1], [Table 2]
|