| |


 |
| Year : 2013 | Volume
: 7
| Issue : 2 | Page : 65-69 |
|
|
|
|
|
ORIGINAL ARTICLE Intramedullary nailing of humeral diaphyseal fractures. Is distal locking really necessary?
Minos Tyllianakis, Pantelis Tsoumpos, Kostas Anagnostou, Anna Konstantopoulou, Andreas Panagopoulos
Department of Shoulder and Elbow Surgery, University Hospital of Patras, Rio, Greece
Correspondence Address:
Andreas Panagopoulos
Department of Shoulder and Elbow Surgery, University Hospital of Patras, Papanikolaou str, 26504 Rio-Patras
Greece
 Source of Support: None, Conflict of Interest: None  | 2 |
DOI: 10.4103/0973-6042.114233

|
|
|
|
| Date of Web Publication | 29-Jun-2013 |
 Abstract Abstract | | |
Purpose: Distal interlocking is regarded as an inherent part of the antegrade humeral nailing technique, but it exposes both the patient and surgeon to radiation, is time consuming, and has a potential risk of damaging neurovascular structures. We have presented our technique of diaphyseal humeral nailing without any distal interlocking in this paper.
Materials and Methods: We have presented a series of 64 consecutive patients (33 male and 31 female, mean age: 41.5 years) with humeral shaft fractures treated with antegrade rigid intramedullary nailing without distal interlocking following a strict intra and postoperative protocol. According to the AO classification, there were 36 type A fractures, 22 type B, and 6 type C. Nails were inserted unreamed or by using limited proximal reaming and they were fitted as snuggly as possible into the medullary canal. After impaction of the nail into the fossa, we carefully tested rotational stability of fixation by checking any potential external rotation when the arm was slightly turned externally and left to the gravity forces. We were ready to add distal screws, but that was not required in these cases. Follow-up assessment included fracture union, complications and failures, and the final clinical outcome at minimum 2-year follow-up using the parameters of the constant score.
Results: All fractures, except two, united between the 4 th and 5 th postoperative month. In one case, nail was exchanged with plate, and, in another, a larger nail was used at a second surgery. Shoulder function according to constant score, at a minimum of 2-year follow-up, was excellent or very good in 93.7% of the patients.
Conclusions: Provided that some technical issues are followed, the method reduces intraoperative time and radiation exposure and avoids potential damage to neurovascular structures.
Keywords: Distal interlocking, humeral fractures, humeral nailing
How to cite this article:
Tyllianakis M, Tsoumpos P, Anagnostou K, Konstantopoulou A, Panagopoulos A. Intramedullary nailing of humeral diaphyseal fractures. Is distal locking really necessary?
. Int J Shoulder Surg 2013;7:65-9 |
 Introduction Introduction | |  |
The advantages of intramedullary nailing (IMN) of acute humeral shaft fractures have been debated since the introduction of this technique. Acute fractures of the humerus have a good healing tendency with non-operative treatment, thanks to the excellent blood supply of the surrounding muscles; thus, functional bracing is still the treatment of choice in many trauma centers. [1],[2] When operative treatment is needed, plate and screws osteosynthesis has been the treatment of choice, [3],[4] and the overall tendency in the actual literature is to give plating a slight advantage over nailing. Very few studies have compared the complications and outcome of nailing versus plating, [5],[6],[7] all having important weaknesses, as there has been no consensus so far regarding either the fundamental principles of the humeral nailing technique (antegrade or retrograde, reamed or unreamed, static or dynamic) as well as to nail types (rigid or elastic) and other important technical aspects. [8],[9]
Distal interlocking is regarded as an inherent part of the humeral nailing technique, but it exposes both the patient and surgeon to radiation while the passage of the locking screws is fraught with danger in a region that concentrates, in a relatively small volume, a multitude of major neurovascular structures. [10],[11],[12] These studies have shown that not only the radial and lateral cutaneous nerve but also the ulnar and median nerve as well as the brachial artery are at high risk when the lateromedial locking technique is applied. Numerous techniques and devices have been proposed to aid distal targeting in long bone fractures, in attempts to overcome some of the associated problems. [13] In humerus especially, the difficulties to obtain a true lateral view, the flattened, and slippery surface of its distal part and the relative narrow holes of the humeral nails are additional problems when a lateromedial approach is selected. [9],[14],[15] Many authors have proposed either an open lateromedial approach for direct vision or the use of anteroposterior screws only.
In our Shoulder and Elbow Department, nailing for acute humeral shaft fractures was introduced 25 years ago as the operative treatment of choice. We have already published good outcomes of antegrade IMN in a large group of selected patients regarding both shoulder function and union rates. [16],[17]
Given the great potential for healing that humeral shaft fractures have, early in our practice, we used in selective cases (not included in this study) no distal interlocking in antegrade humeral nailing in order to reduce intraoperative time and potential complications and unnecessary exposure to radiation. Following accurate measurement of nail length, the nail was impacted 1-2 cm proximal to the olecranon fossa, at the cone-shaped diaphyseal flute of the distal humerus, ensuring rotational stability distally to the fracture area. No effort was made for a press fit application of the nail, as, in most cases, the nails were of small diameter. After the first encouraging results, we used this method in most cases of humeral fractures following a simple yet strict intraoperative and postoperative protocol. To our knowledge, this is the first report of antegrade humeral nailing, using solely rigid nails, without distal interlocking.
 Materials and Methods Materials and Methods | |  |
In 1999, the senior author (M.T.) set off to use proximally locked only IMN for acute fractures of the shaft of the humerus. All patients who presented to our Emergency Department with an acute humeral shaft fracture between the beginning of 2000 and the end of 2009 and who underwent IMN were included in this study. Patient demographics and baseline characteristics were prospectively recorded: Gender, age, accident type, and energy level of trauma, localization of the fracture, fracture classification, concomitant injuries, intra- and postoperative complications including nerve palsies, length of hospital stay, and delayed union and non-union. Delayed union was defined as the failure of healing after 14 weeks and non-union as failure of healing after 24 weeks. On follow-up, all available patients were examined by two independent observers P.T. and A.K. Patients were interviewed concerning pain and shoulder mobility. Shoulder function was assessed in accordance with the constant score. The upper arm was X-rayed in two planes to confirm fracture healing and integrity of implants. The assessments of function were made at the latest postoperative visit, at a minimum of 2 years. From 2000 to 2009, 69 patients were treated with this method in our department. Exclusion criteria were young patients in whom growth plates were open, pathological fractures, non-unions or delayed unions, and fractures with preoperative radial nerve palsy whenever surgical treatment was indicated by the fracture type (except one polytrauma patient with radial nerve avulsion). Three patients missed the final follow-up and two died for reasons unrelated to the fracture, leaving 64 patients for the study. There were 33 male and 31 female with a mean age of 41.5 years (age range: 17-76). Traffic accident was the mechanism of injury in 39 cases and a fall from height in the rest. Twenty-one patients (33%) had multiple other injuries. There were 29 left-sided humeral fractures and 35 right-sided ones. Nineteen fractures (30%) were localized in the proximal third, 32 (50%) in the middle, and 13 (20%) in the distal third. A minimum length of 3-4 cm of the distal fragment was considered necessary for stable fixation. According to the OTA classification, [18] there were 36 type A, 22 type B, and 6 type C fractures. Especially in the last category (C), there were 4 segmental fractures (C2) and 2 comminuted (C1) fractures. Open fractures were also included (3 in these series) regardless of their degree according to Gustilo and Anderson classification.
The nails we used were always of the rigid type (UHN, Synthes and Russel-Taylor, Smith and Nephew, Richards) and had a diameter of 7 or 8 mm. Two different techniques of proximal nail insertion were used according to the type of the nail. At the final follow-up, no clinical differences of shoulder function were noted regarding the type of entry point. For the Russel-Taylor nail (34 cases), a modified extra rotator cuff entry point was used just 1 cm below the greater tuberosity. [17] The nail was inserted after minimal (4 cm) proximal reaming. For the UHN (30 cases), insertion was made after 1 cm incision of the rotator cuff, 1 cm medially to cuff insertion. Rotator cuff was repaired with a few sutures at the end of operation. In all cases, a small 2-cm incision was done at the fracture site and a finger was used to reduce the fracture. This maneuver not only facilitated nail insertion into the distal part of the humerus but also made sure that no soft tissues and nerves in particular were entrapped at the fracture site. Nails were inserted unreamed in the distal part and they were fitted as snuggly as possible into the medullary canal. In any case, the nail was slightly impacted into the distal part (1-2 cm). This impaction of the nail in the narrow distal medullary canal was very important, provided that an accurate measurement of nail length has been made. One proximal screw was inserted with a proper targeting device according to the technical guidelines of each nail. Intraoperative fluoroscopy was used to check entry point of the nail, fracture site, distal part of the nail, and proximal screws placement. The mean operation time was 70 min (range: 55-110).
Postoperatively, the arm was suspended in an envelope sling and the patient was advised to flex the ipsilateral elbow from the first postoperative day as many times a day as possible. Strict advice was given against any attempt at external rotation of the arm for the first 4 weeks. Sling was disregarded after a month, and the patient started active external rotation along with muscle strengthening exercises. At 6 weeks, exercises to improve external rotation were initiated that usually lasted for 2-3 weeks. Assisted forward flexion of the shoulder was encouraged from day 1 with care not to perform simultaneous external rotation of the affected arm. Further mobilization of the shoulder was done according to a protocol for cuff tear repair.
 Results Results | |  |
No infections or postoperative nerve palsies were noted. Patients stayed for an average of 7 days in the hospital (range: 3-19 days). In four patients, a nail of inappropriate length was used. In one case, it was too long, causing proximal protrusion and diastasis at the fracture site. It was exchanged with a compression plate 8 weeks postoperatively, as there was no sign of callus in the radiographs. In three other patients, the nail was too short and inserted deeply into the humeral head. A polytrauma patient with open grade III B fracture (avulsion of the radial nerve) was treated with a too narrow nail. The patient remained intubated in the ICU, and, after a month, the nail was exchanged with a larger one that was placed without any locking screws since callus formation was already apparent in the radiographs. At the same surgery, tendon transfer for radial nerve palsy was performed.
Patients were routinely reexamined at 3, 6, and 12 weeks and at 6 months. If three cortices appeared united at 12 weeks, the patient was allowed use of the limb freely, otherwise it was postponed until final examination. All fractures united by 4-5 months. By that time, all patients had regained their preoperative range of motion of the shoulder and elbow. No patient required additional physiotherapy done by an expert. Mean follow-up period was 6.5 years (range: 2-10 years). Using the constant score, 52 patients had an excellent shoulder function (81.2%), 8 patients very good (12.5%), 2 patients fair (3.1%), and 2 poor (3.1%). [Figure 1], [Figure 2], [Figure 3] and [Figure 4] show different types of humeral shaft fracture and the final radiological and clinical evaluation. As our policy is not to remove any implant from the upper limb unless specific indications exist, nail removal after union was not done to any patient.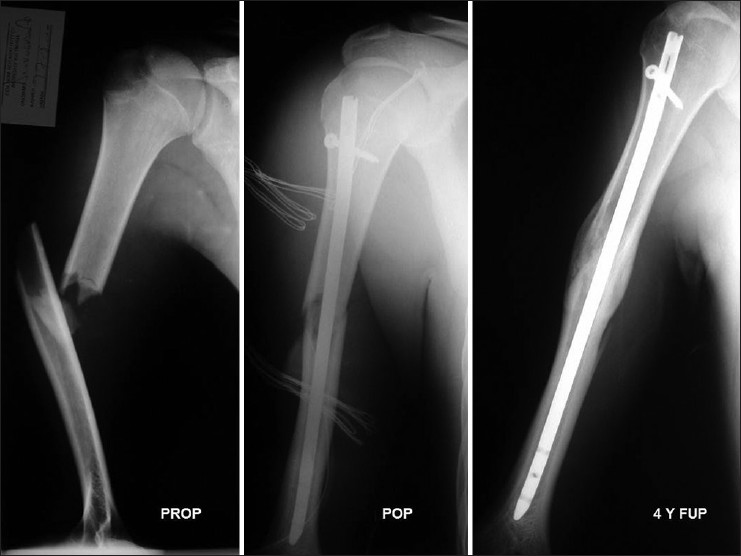 | Figure 1: Preoperative and postoperative X-ray of a midshaft humeral fracture (OTA type 12-B2) in a 17-year-old patient involved in a traffic accident. Four years postoperatively, there was solid callus formation
and the constant score was 100 (excellent)
Click here to view |
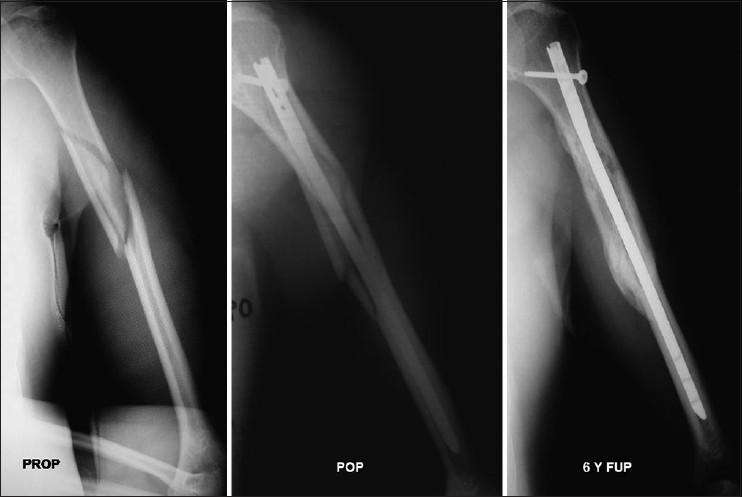 | Figure 2: Preoperative and postoperative X-ray of a humeral shaft fracture extended to proximal third of the diaphysis (OTA type 12-B1) in a 60-year-old patient after a fall of his height. Despite the extended comminution, the nail was impacted at the distal part and led to uneventful healing of the fracture. The constant score at 6 years postoperatively was 95
Click here to view |
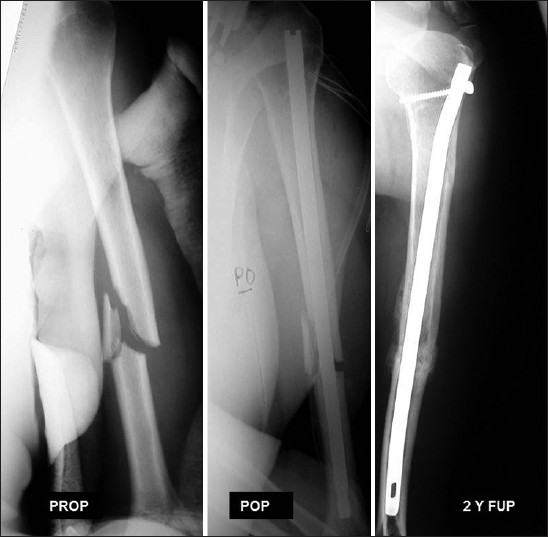 | Figure 3: Preoperative and postoperative X-ray of a humeral shaft fracture extended to distal third of the diaphysis (OTA type 12-B2) in a 23-year-old patient after a fall from height. Despite the 1 cm diastasis at the fracture site, healing was achieved as soon as 3 months postoperative. The 2-year follow-up showed solid callus and a constant score of 94
Click here to view |
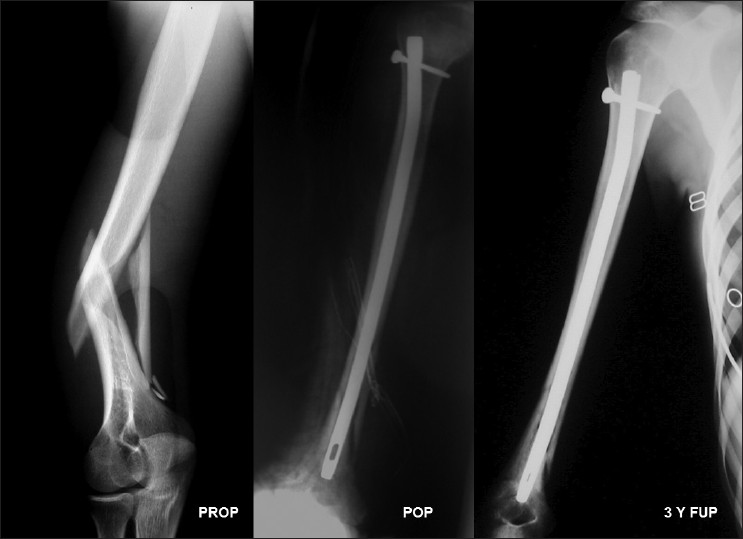 | Figure 4: Preoperative and postoperative X‑ray of a humeral shaft fracture extended to the distal third of the diaphysis (OTA type 12‑B1) in a 22‑year‑old patient involved in a traffic accident. Excellent radiological result was seen 3 years postoperatively. The constant score was 95 at the last follow‑up
Click here to view |
 Discussion Discussion | |  |
Both locking nailing and locking plating are methods of choice for fractures of the proximal and middle third of the humerus. A large series [19] failed to find any significant difference between the two methods in fractures of the proximal third. Likewise, a meta-analysis comparing compression plates with locking nails for humeral shaft fractures did not reveal superiority of one method over the other. The same study showed that the risk of reoperation and shoulder impingement might be higher with nails, but evidence was inconclusive. [20] Again, similar results were found for fractures of the middle third treated with rigid antegrade or retrograde nailing, the latter proposed for patients with wide medullary canal and preexisting shoulder problems. [21]
The main problems of antegrade nailing for humeral fractures are three: Violation of the rotator cuff, soft tissue injury around the shoulder, and distal locking. Modifications of the surgical technique with sophisticated nail designs have been proposed in order to overcome problems of the cuff, but no further studies have validated these proposals. [17],[22],[23] It should be noted though that shoulder dysfunction may also occur after conservative treatment or plating or retrograde nailing. [2],[24],[25],[26] Delicate tissues are vulnerable at the insertion of proximal screws, as indicated by many studies. [27],[28],[30] Nails that do not use proximal locking have been proposed, but they are associated with less stability and are considered more effective if their entry portal is closer to the fracture site. [8],[9] Proximal and distal locking are integral elements for rotational stability of an IMN. Yet distal locking is associated with some problems: Lateral view of the humerus is not easily obtained, locking holes are narrow, the lateral surface of the humerus is "slippery" and the danger of injury to the radial nerve and other vulnerable structures lurks. [8],[9],[31] Success of commercial targeting devices is still inconsistent.
Since it seems that little can be done to solve problems of distal locking, we tried, if possible, to skip it. In our first cases (not included in the series), we found that the nail can be impacted into the distal humerus, which has a cone shape configuration of the distal medullary canal. That impaction along with snug insertion of the nail provided some initial intraoperative stability. On the other hand, a standing person performs elbow flexion with the arm in 30° to 45° of internal rotation. Therefore, when a patient is advised postoperatively to flex the elbow, he/she does it in the same direction, thus protecting it from unnecessary external rotation. Recommendation against external rotation is easily followed by the patient as it causes pain. The authors think that muscle exercises with frequent elbow flexion enhance healing of the fracture by applying further compression at the fracture site. By the end of 4 weeks, fibrous callus has been formed and the patient is allowed to move the arm more freely.
It must be mentioned though that this technique is deceptively easy. Two issues require particular attention. Proper length of the nail is critical because too short nail may not allow impaction into the distal part or lead to deep insertion of the nail into the humeral head, rendering potential removal of the nail extremely difficult. On the other hand, too long nail may keep the fracture ends apart and cause impingement of the shoulder. The effort to insert the nail snuggly in order to increase stability requires particular attention as it may protrude into the olecranon fossa or may cause iatrogenic fracture or propagation of the fracture. We do not use any preoperative landmarks for the calculation of the accurate length of the nail. The use of a second guide rod of the same length facilitates measurement, and the length is estimated taking into account the type of the fracture and especially the presence of fracture gap before nail application. Usually, a slightly shorter nail is better as this can be inserted a little bit deeper in the humeral head. The new designed nails (Smith-Nephew) have a special measurement device that can estimate the appropriate length with great accuracy. There is no doubt that, with proximal and distal locking, the patient can regain almost full range of motion soon after surgery as stability has been secured. On the contrary, patients in our series had some restriction regarding postoperative mobilization. However, our results are comparable to those of other series with IMN of the humerus. [32]
The interesting finding of this study is that, except for the patients with the complications mentioned before, all other fractures healed uneventfully. In contrast to recent biomechanical studies, [33] which have shown that non-interlocked nails are inferior to interlocked ones in rotationally unstable humeral fractures, the proposed method seems to be a promising operative procedure regarding union rates, reduction of operative time, radiation exposure, and iatrogenic nerve injury, but some limitations still exist. The study was retrospective, without control group and concerned a relatively small number of patients, but one must consider the healing ability of humerus when treated conservatively and the small percentage of patients who finally need surgical intervention. Other weak points include the potential failure of fixation stability, the need of technical expertise, and the restriction in postoperative mobilization. A biomechanical testing of rotational stability and bending stiffness in cadaver humeri, which is ongoing in our department will probably attest the good clinical outcome of the proposed technique.
 References References | |  |
| 1. | Bleeker WA, Nijsten MW, ten Duis HJ. Treatment of humeral shaft fractures related to associated injuries. A retrospective study of 237 patients. Acta Orthop Scand 1991;62:148-53. 
[PUBMED] |
| 2. | Wallny T, Westermann K, Sagebiel C, Reimer M, Wagner UA. Functional treatment of humeral shaft fractures: Indications and results. J Orthop Trauma 1997;11:283-7. 
[PUBMED] |
| 3. | Vander Griend R, Tomasin J, Ward EF. Open reduction and internal fixation of humeral shaft fractures. Results using AO plating techniques. J Bone Joint Surg Am 1986;68:430-3. 
[PUBMED] |
| 4. | Heim D, Herkert F, Hess P, Regazzoni P. Surgical treatment of humeral shaft fractures--the Basel experience. J Trauma 1993;35:226-32. 
[PUBMED] |
| 5. | Chapman JR, Henley MB, Agel J, Benca PJ. Randomised prospective study of humeral shaft fracture fixation: Intramedullary nails versus plates. J Orthop Trauma 2000;14:162-6. 
[PUBMED] |
| 6. | Changulani M, Jain UK, Keswani T. Comparison of the use of the humerus intramedullary nail and dynamic compression plate for the management of diaphyseal fractures of the humerus. A randomised controlled study. Int Orthop 2007;31:391-5. 
[PUBMED] |
| 7. | McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Joint Surg Br 2000;82:336-9. 
[PUBMED] |
| 8. | Garnavos C. Humeral nails: When to choose what and how to use. Curr Orthop 2005;19:294-304. 
|
| 9. | Garnavos C. Diaphyseal humeral fractures and intramedullary nailing: Can we improve outcomes? Indian J Orthop 2011;45:208-15. 
[PUBMED]  |
| 10. | Rupp RE, Chrissos MG, Ebraheim NA. The risk of neurovascular injury with distal locking screws of humeral intramedullary nails. Orthopedics 1996;19:593-5. 
[PUBMED] |
| 11. | Blyth MJ, Macleod CM, Asante DK, Kinninmonth AW. Iatrogenic nerve injury with the Russell-Taylor humeral nail. Injury 2003;34:227-8. 
[PUBMED] |
| 12. | Noger M, Berli MC, Fasel JH, Hoffmeyer PJ. The risk of injury to neurovascular structures from distal locking screws of the Unreamed Humeral Nail (UHN): A cadaveric study. Injury 2007;38:954-7. 
[PUBMED] |
| 13. | Whatling GM, Nokes LD. Literature review of current techniques for the insertion of distal screws into intramedullary locking nails. Injury 2006;37:109-19. 
[PUBMED] |
| 14. | Moran MC. Distal interlocking during intramedullary nailing of the humerus. Clin Orthop Relat Res 1995;317:215-8. 
[PUBMED] |
| 15. | Kolonja A, Vecsei N, Mousani M, Marlovits S, Machold W, Vecsei V. Radial nerve injury after anterograde and retrograde locked intramedullary nailing of humerus. A clinical and anatomical study. Osteo Trauma Care 2002;10:197-99. 
|
| 16. | Dimakopoulos P, Papas M, Kaisidis A, Panagopoulos A, Lambiris E. Antegrade intramedullary nailing in humeral shaft fractures. Osteo Trauma Care 2003;11:S58-63. 
|
| 17. | Dimakopoulos P, Papadopoulos AX, Papas M, Panagopoulos A, Lambiris E. Modified extra rotator-cuff entry point in antegrade humeral nailing. Arch Orthop Trauma Surg 2005;125:27-32. 
[PUBMED] |
| 18. | Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium-2007: Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 2007;21(Suppl 10):S1-133. 
|
| 19. | Gradl G, Dietze A, Kääb M, Hopfenmüller W, Mittlmeier T. Is locking nailing of humeral head fractures superior to locking plate fixation? Clin Orthop Relat Res 2009;467:2986-93. 
|
| 20. | Bhandari M, Devereaux PJ, McKee MD, Schemitz EH. Compression plating versus intramedullary nailing of humeral shaft fractures--A meta-analysis. Acta Orthop 2006;72:279-84. 
|
| 21. | Cheng HR, Lin J. Prospective randomized comparative study of antegrade and retrograde locked nailing for middle humeral shaft fracture. J Trauma 2008;65:94-102. 
[PUBMED] |
| 22. | Park JY, Pandher DS, Chun JY, Md ST. Antegrade humeral nailing through the rotator cuff interval: A new entry portal. J Orthop Trauma 2008;22:419-25. 
[PUBMED] |
| 23. | Stannard JP, Harris HW, McGwin G Jr, Volgas DA, Alonso JE. Intramedullary nailing of humeral shaft fractures with a locking flexible nail. J Bone Joint Surg Am 2003;85:2103-10. 
[PUBMED] |
| 24. | Ekholm R, Tidermark J, Törnkvist H, Adami J, Ponzer S. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma 2006;20:591-6. 
|
| 25. | Flinkkilä T, Hyvönen P, Siira P, Hämäläinen M. Recovery of shoulder joint function after humeral shaft fracture: A comparative study between antegrade intramedullary nailing and plate fixation. Arch Orthop Trauma Surg 2004;124:537-41. 
|
| 26. | Rosenberg N, Soudry M. Shoulder impairment following treatment of diaphyseal fractures of humerus by functional brace. Arch Orthop Trauma Surg 2006;126:437-40. 
[PUBMED] |
| 27. | Bono CM, Grossman MG, Hochwald N, Tornetta P 3 rd . Radial and axillary nerves. Anatomic considerations for humeral fixation. Clin Orthop Relat Res 2000;373:259-64. 
|
| 28. | Albritton MJ, Barnes CJ, Basamania CJ, Karas SG. Relationship of the axillary nerve to the proximal screws of a flexible humeral nail system: An anatomic study. J Orthop Trauma 2003;17:411-4. 
[PUBMED] |
| 29. | Evans PD, Conboy VB, Evans EJ. The Seidel humeral locking nail: An anatomical study of the complications from locking screws. Injury 1993;24:175-6. 
[PUBMED] |
| 30. | Lin J, Hou SM, Inoue N, Chao EY, Hang YS. Anatomic considerations of locked humeral nailing. Clin Orthop Relat Res 1999;368:247-54. 
[PUBMED] |
| 31. | Garnavos C. Intramedullary nailing for humeral shaft fractures: The misunderstood poor relative. Curr Orthop 2001;15:68-75. 
|
| 32. | Rommens PM, Kuechle R, Bord T, Lewens T, Engelmann R, Blum J. Humeral nailing revisited. Injury 2008;39:1319-28. 
[PUBMED] |
| 33. | Blum J, Karagül G, Sternstein W, Rommens PM. Bending and torsional stiffness in cadaver humeri fixed with a self-locking expandable or interlocking nail system: A mechanical study. J Orthop Trauma 2005;19:535-42. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
|
