| |


 |
| Year : 2013 | Volume
: 7
| Issue : 2 | Page : 70-78 |
|
|
|
|
|
REVIEW ARTICLE Reverse shoulder arthroplasty in acute fractures of the proximal humerus: A systematic review
Stig Brorson1, Jeppe V Rasmussen1, Bo S Olsen1, Lars H Frich2, Steen L Jensen3, Asbjřrn Hróbjartsson4
1 Department of Orthopaedic Surgery, Herlev University Hospital, Herlev, Denmark
2 Department of Orthopaedic Surgery, Odense University Hospital, Rigshospitalet, Denmark
3 Department of Orthopaedic Surgery, Aalborg University Hospital, Rigshospitalet, Denmark
4 Department of Orthopaedic Surgery, The Nordic Cochrane Centre, Rigshospitalet, Denmark
Correspondence Address:
Stig Brorson
Department of Orthopaedic Surgery, Herlev University Hospital, Herlev Ringvej 75, 2730 Herlev
Denmark
 Source of Support: The first author was supported by a grant from The Danish Agency for Science, Technology, and Innovation, Conflict of Interest: None  | 14 |
DOI: 10.4103/0973-6042.114225

|
|
|
|
| Date of Web Publication | 29-Jun-2013 |
 Abstract Abstract | | |
The indications for surgical intervention in complex fractures of the proximal humerus are disputed. In elderly patients with poor bone stock it may be impossible to obtain satisfactory fixation of the tuberosities to a hemiarthroplasty (HA). In such cases primary insertion of a reverse shoulder arthroplasty (RSA) has been suggested. We aimed to review clinical studies reporting benefits and harms of RSA in acute fractures. A systematic review. We included 18 studies containing 430 RSA in acute fractures. We found no randomized clinical trials. Four studies compared outcome after RSA with a historical control group of HA. The median constant score was 58 (range 44-68) which is comparable to previous reviews of HA in 4-part fractures. Complications included dislocation, infection, hematoma, instability, neurological injury, reflex sympathetic dystrophy, intraoperative fractures, periprosthetic fractures, and baseplate failure. Scapular notching was reported in 11 studies with a median value of 25% (range 0-94). Heterogeneity of study designs and lack of primary data precluded statistical pooling of data. No high quality evidence was identified. Based on the available evidence the use of RSA in acute fractures is questionable. The complication rate was high and the clinical implications of long term scapular notching are worrying. Randomized studies with long term follow up using the latest techniques of tubercular reinsertion in RSA toward HA should be encouraged.
Keywords: Proximal humeral fractures, proximal humerus fractures, reverse shoulder arthroplasty, reverse shoulder prosthesis, tuberosity fixation
How to cite this article:
Brorson S, Rasmussen JV, Olsen BS, Frich LH, Jensen SL, Hróbjartsson A. Reverse shoulder arthroplasty in acute fractures of the proximal humerus: A systematic review. Int J Shoulder Surg 2013;7:70-8 |
 Introduction Introduction | |  |
The indications for surgical intervention in complex fractures of the proximal humerus are controversial. [1],[2],[3] In most centers the treatment of choice for displaced 4-part fractures, fracture-dislocations, and head-splitting fractures is primary hemiarthroplasty (HA). Acceptable pain relief has been reported in primary HA but so has marked limitation in function [4] and results are often compromised by secondary displacement of the tuberosities. [5] In elderly patients with poor bone stock it may be impossible to obtain satisfactory fixation and healing of the tuberosities. In such cases primary insertion of a reverse shoulder arthroplasty (RSA) has been suggested as an effective and safe treatment option. [6],[7],[8],[9],[10]
The modern concept of RSA was developed by Grammont in 1985 based on prior experiences with constrained designs. [11],[12],[13] However, the design did not appear in the scientific literature until the paper by Grammont and Baulot in 1993. [14] Initially, it was developed for arthritic shoulders with severe destruction of the rotator cuff. However, Grammont himself used RSA for acute fractures and fracture sequelae in an unpublished series of 22 cases from 1989 to 1993. [15] Clinical series of RSA for acute fractures were initiated in France in 1993 [16] and in 2003 the RSA was approved by the American Food and Drug Administration for use in severe cuff arthropathy, failed HA, osteoarthritis, and irreducible 3- and 4-part fractures of the proximal humerus. [17]
In RSA the deltoid muscle is utilized as a compensation for the deficient rotator cuff by creating a stable center of rotation in the glenoid allowing for active flexion and abduction of the arm. The deltoid function is enhanced by moving the center of rotation distally and medially increasing the tension of the deltoid fibers and decreasing the mechanical torque at the glenoid component. [18] In displaced 4-part fractures and fracture-dislocations some forward elevation can be obtained even if the tuberosities do not heal. However, in such cases poor rotation can be expected. New techniques of tuberosity fixation have been proposed and results have been encouraging. [19],[20],[21],[22],[23]
Short term pain relief and early mobilization after RSA in acute fractures has been reported, [7],[10],[24],[25] but only few long-term results have been published. [16],[22] Long operator learning curves for RSA in shoulder arthritis have been reported, [26],[27] and revision surgery is challenging. [28],[29] Reported complications to RSA include dislocation, infection, hematoma, instability, loss of rotation, neurological injury, reflex sympathetic dystrophy, intraoperative fractures, peri-prosthetic fractures, baseplate failure and scapular notching. [18],[29],[30],[31],[32],[33]
In France and the U.S., RSA is commonly used for complex fractures of the proximal humerus and RSA is considered a useful option worldwide. Thus, the overall balance of the benefits and harms of this fairly new surgical procedure in proximal humeral fractures is unclear. We have been unable to identify any systematic review studying outcome after RSA in acute fractures. We therefore decided to systematically search and review clinical studies reporting benefits and harms of RSA in acute fractures of the proximal humerus.
 Methods Methods | |  |
We included randomized clinical trials, observational studies, and case series having included at least 10 acute fractures treated with RSA. We included studies without language restriction. All patients should be followed up for at least 6 months. We excluded studies evaluating results after RSA for other indications (cuff arthropathy, revision surgery, delayed fracture management, tumor surgery). We searched Pubmed and Cochrane Library (November 7 th 2011) using the search terms:
(inverse* OR reverse* OR delta* OR grammont* OR inverted*) AND ((shoulder* OR humer*) AND (fractu* OR broken* OR break*) OR ("Shoulder Fractures"[Mesh])).
We further searched Embase, Web of Science, and abstracts and posters from the annual meetings of SECEC (Société Européenne de Chirurgie de l'Epaule et du Coude) from 2009 to 2011.
One author conducted the literature search and scanned all references for eligibility. Articles that could not clearly be excluded were retrieved in full text and read independently by two authors who decided independently on eligibility. Disagreements were resolved by discussion. Study characteristics and results were extracted independently by two authors using pre-tested forms. In cases of discrepancies between data in abstract and text we extracted data from the most comprehensive source. In cases of multiple publication of data from identical patients at different follow-up we summarized the temporal development and included data from the most recent follow-up only. We did not contact the authors for primary patient data. Data were summarized in a table organized according to the study design.
The risk of bias in observational studies was assessed according to pre-defined criteria: (1) cohort clearly defined at baseline, (2) cohort consecutively or randomly sampled, (3) number of drop-outs or loss to follow-up accounted for, (4) outcome blindly assessed, and (5) conflicts of interests declared. [34],[35],[36]
 Results Results | |  |
We identified 190 articles by the internet search, 64 were clearly not relevant, 126 were reviewed in full text [Figure 1]. One hundred and eight of those did not comply with the inclusion criteria. Thus, we included 18 clinical studies containing 430 RSA in acute fractures [Table 1]. There were no randomized clinical trials, four retrospective cohort studies with historical control groups, [22],[24],[37],[38] four prospective cohort studies, [8],[9],[39],[40] six retrospective cohort studies, [7],[10],[19],[21],[23],[41] and four cohort studies with unclear designs. [6],[16],[42],[43] Ten studies were conducted in France.
The studies were reported as conference abstracts, [19],[21],[41],[44] posters, [6],[7],[9],[39],[43] and full articles. [8],[10],[16],[24],[37],[38],[39],[40],[42] The median number of patients included per study was 20 (range 10-47). Fourteen studies reported outcome as non-adjusted constant score (CS), two studies [41],[43] used adjusted CS only, and two studies [10],[38] used other outcome measures. The median non-adjusted CS was 58 (range 44-68). Two studies [22],[37] did not report complication data. The quality of the studies was generally low. Only one study [42] complied with all five pre-defined items. Two studies [16],[24] complied with four out of five items. Six studies did not comply with any of the five pre-defined items. [6],[7],[8],[21],[23],[43]
Cohort studies with historical control
Gallinet et al.[24] retrospectively followed a cohort of 16 patients with 3- and 4-part fractures for 6-18 months (mean age 74). Outcome was compared with a control group of 17 patients treated with HA (mean age of 74) and a follow-up of 6-55 months. One patient underwent tuberosity reattachment. Mean CS was 53 (range 34-76) in the RSA group compared to 39 (range 19-61) in the HA group. The difference was statistically significant (P = 0.005). Complications in the RSA group included one deep infection and one reflex sympathetic dystrophia. Scapular notching was found in 15 radiographs.
Reitman and Kerzhner [37] retrospectively followed a cohort of 13 patients with 3- and 4-part fractures (including six fracture-dislocations) for 8-46 months (mean age 70). Five patients underwent tuberosity reattachment. Outcome was compared with a historical control group of 112 HA from three studies on fractures of "equivalent severity." Mean CS was 67 (range 45-77) in the RSA group compared to 84 in the HA group. Statistically testing was not reported. Complications in the RSA group included two axillary nerve palsies, one radial nerve palsy, and one hematoma. Scapular notching was found in three radiographs.
Sirveaux et al.[22] retrospectively followed a cohort of 11 3- and 4-part fractures for 46 months (range 24-109). Mean age was 78 years. All patients underwent tuberosity reattachment. Outcome was compared to a historical control group of 139 HA from a multicenter study. Mean CS was 55 (range 31-73) in the RSA group compared to 51 in the HA group. The difference was reported as not statistically significant. Complications in the RSA group included one dislocation, one glenoid migration, four non-unions of the greater tuberosity, and six non-unions of the lesser tuberosity. Scapular notching was not reported.
Young et al.[38] retrospectively compared 10 RSA in patients with 3- and 4-part fractures (mean age 77) to 10 HA (mean age 75) with a follow-up of 22-44 months. Five patients underwent reattachment of both tuberosities, four underwent greater tuberosity reattachment, and both tuberosities were excised in one patient. ASES (American Shoulder and Elbow Surgeons) score was 65 (range 40-88) in the RSA group and 67 (26-100) in the HA group. Oxford shoulder score was 29 (range 15-56) and 22 (range 12-34) respectively. Statistically testing was not reported and no complications were reported in the RSA group. Scapular notching was found in two radiographs.
Prospective cohort studies
Klein et al.[8] followed a cohort of 20 AO (Arbeitsgemeinschaft für Osteosynthesefragen) type B and C fractures for 33 months (range 24-52). Mean age was 75 years and mean CS was 68 (range 47-98). Dordain et al.[39] followed a consecutive cohort of 20 3- and 4-part fractures for 17 months (range 12-32). Mean age was 80 years and mean CS was 59 (range 47-98). Reuther et al.[9] followed a consecutive cohort of 44 3- and 4-part fractures for 14 months (range 5-28). Mean age was 80 years and mean CS was 58. Terragnoli et al.[40] followed a cohort of 18 3- and 4-part fractures for 6 months. Mean age was 75 years. Mean CS was 59.
Retrospective cohort studies
Gallinet et al.[19] retrospectively reviewed a cohort of 40 patients for 23 months. Mean age was 76. CS was used, but the values were not reported. Grisch et al.[45] retrospectively reviewed a cohort of 24 3- and 4-part fractures for 23 months (range 12-60). Mean age was 80, and mean CS was 66 (34-83). Hubert et al.[41] retrospectively reviewed a cohort of 14 3- and 4-part fractures for 14 months. Mean age was 80 and weighted CS was 80%. Lenarz et al.[10] retrospectively reviewed 30 patients with 3- and 4-part fractures for 23 (12-36) months. Mean age was 77. Mean ASES score was 78 (36-98). Russo et al.[21] retrospectively followed a cohort of 16 3- and 4-part fractures for 14 months. Mean age was 74 years. A new tuberosity fixation technique was used in nine out of the 16 cases. CS was 68 in usual tuberosity fixation compared to 90 in the new tuberosity fixation group (statistically testing not reported). Sirveaux et al.[23] retrospectively followed a cohort of 47 fractures for 30 months. Mean age was 79, and mean CS was 55. They reported that healing of the greater tuberosity affected CS (57 compared to 41, statistical testing not reported).
Prospective or retrospective cohort studies (design unclear)
Bufquin et al.[42] reviewed a consecutive series of 43 3- and 4-part fractures for 22 months (range 6-58). Mean age was 78, and mean CS was 44 (range 16-69). Emily et al.[43] reviewed a consecutive series of 15 3- and 4-part fractures for a mean of 18 months. Mean age was 78, and mean adjusted CS was 45 in patients with no external rotation compared to mean adjusted CS of 98 in patients with at least 10° of external rotation (statistical testing not reported). George et al.[6] reviewed a consecutive series of 19 fractures (Duparc type 3 or 4) for 36 months. Mean age was 81, and mean CS was 58. The cohort by Cazeneuve and Cristofari [Table 2] was established in 1993 and the most recent follow-up was in 2011. [16] Outcome has been reported in several publications [16],[46],[47],[48],[49],[50],[51] and the cohort has been continuously enlarged. Data from the most recent follow-up were included. They reviewed 35 patients with RSA (24 fractures and 11 fracture-dislocations) for 1-17 years. Mean CS was 53. Limited rotation preventing eating, dressing, and body hygiene was reported. 60% had abnormal radiographs after 7 years.
 Discussion Discussion | |  |
We included 18 clinical studies with a high risk of bias and no randomized clinical studies. Mean CS after RSA in comparative studies ranged from mean CS 53-67 compared to 39-84 in HA. Numerous complications after RSA were reported including dislocation, infection, hematoma, instability, neurological injury, reflex sympathetic dystrophy, intraoperative fractures, periprosthetic fractures, and baseplate failure. Scapular notching was reported in 11 out of 18 studies with a median value of 25% (range 0-94) [Table 3].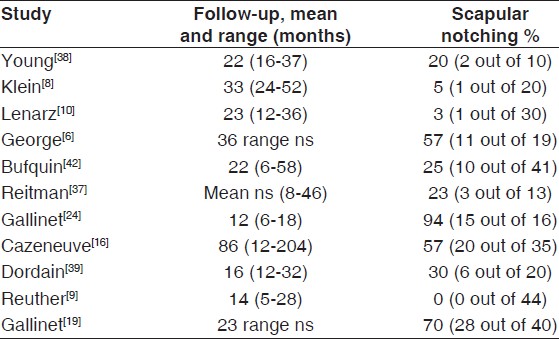 | Table 3: Scapular notching after reverse shoulder arthroplasty in acute fractures
Click here to view |
We conducted an iterative search in several databases and identified more studies than any previous reviews. The weakness of our study is the lack of high quality evidence precluding pooling of outcome data.
We have been unable to identify any previous systematic reviews of outcome after RSA in acute fractures of the proximal humerus. A narrative review by Spencer and Voloshin [52] included four short-term studies that reported an active elevation of 97° to 122° and a complication rate of 15%-28%. Four studies included in our review compared outcome after RSA with outcome from a historical control group of HA. The reported outcome was comparable to previous systematic reviews of outcome after HA in 4-part fractures. Thus, den Hartog et al.[53] reported a mean CS of 55 (SD = 9.6) in 258 HA. Kontakis et al.[4] reported a mean CS of 57 (range 11-98) in 560 primary HA. The heterogeneity of study designs and lack of primary patient data precluded a prudent pooling of data. Three descriptive studies, [6],[42],[43] but no comparative studies, reported individual patient data.
Selection bias may occur if patients with the most severe pathology are selected for RSA. Several authors did not clearly report their criteria for using RSA, and baseline characteristics may differ between the studies. The cohort was clearly defined at baseline in eight studies. [10],[16],[22],[24],[37],[38],[41],[42] Only three studies reported a cohort consecutively or randomly sampled suggesting a high-risk of selection bias. [16],[24],[42] To eliminate selection bias clinical trials including, randomization and concealment of allocation are warranted.
Follow-up time for RSA in comparative studies ranged from 6 months to 109 months compared with follow up for HA ranging from 6 months to 70 months. Mean follow-up time was longer for HA compared with RSA in three out of four comparative studies. In the fourth study, follow-up time was matched. [37] A statistically significant difference in follow-up time was reported in one study. [22] Short follow-up for RSA may lead to overestimation of outcome as long-term complications may occur.
In only five studies outcome was assessed by an independent observer. Poolman et al. [54] reported that in orthopedic studies with continuous outcome measures, un-blinded outcomes assessment was associated with significantly larger treatment effects than blinded outcomes assessment (standardized mean difference, 0.76 compared with 0.25; P = 0.01). In studies with dichotomous outcomes, un-blinded outcomes assessments were associated with significantly greater treatment effects than blinded outcomes assessments (odds ratio, 0.13 compared with 0.42; P < 0.001). Similarly, we have reported that non-blinded assessors of subjective binary outcomes generate substantially biased effect estimates in randomized clinical trials, exaggerating odds ratios by 36%. [55]
A change in surgical procedure has taken place in the included studies. RSA was originally used in cases when reconstruction of the tuberosities was impossible. However, reconstruction of the tuberosities seems to improve stability, and good functional outcome has been reported in cases where tuberosity fixation in RSA was performed. [21],[23],[43],[56] Sirveaux et al.[23] reported a mean CS of 57 if the greater tuberosity was healed compared to 41 if the greater tuberosity was not healed. Emily et al.[43] reported a mean adjusted CS of 45 in patients with no external rotation compared to 98 in patients with at least 10° of external rotation. They concluded that fixation of the greater tuberosity is essential for restoring external rotation. The mean active external rotation values were reported in nine studies [Table 4]. The median value was 20° (range 9-49). If, however, tuberosity fixation is possible, a conventional prosthesis may represent a less expensive solution.
The surgical approaches reported were superolateral or lateral deltosplit in eight studies, anterosuperior in one study, and deltopectoral in six studies. In three studies, the surgical approach was unclear. Three studies used more than one approach. It was not possible to correlate the clinical outcome to the surgical approach from the published data. Only three studies provided data on the surgeons' experience and it was not possible to compare clinical outcome with the surgeons' experience from the published data. No data on the number of RSA performed at each center were available. Recently published data on learning curve in RSA have suggested that 18 RSA should be inserted by high volume surgeons before the operation time stabilizes. [26] However, no data on the clinical implications of learning curve for the patient was reported.
Most authors do not recommend the use of RSA in younger patients. However, a closer look at the 12 studies reporting range of age reveals that three studies included patients younger than 60 and eight studies included patients younger than 70. Reporting of non-adjusted CS was preferred whenever possible because age- and sex-adjusted CS seems to favor outcome in the very elderly.
Reflex sympathetic dystrophy was reported in 6 cases; neurological complications in 9 cases; intraoperative fractures in 5 cases; dislocations in 7 cases; infections in 5 cases, and intraoperative fractures in 5 out of the 430 cases. The complications rates, however, were likely underreported as several studies surprisingly reported no complications at all after RSA. Scapular notching is a complication unique to RSA. It may occur in adduction if the polyethylene component of the humeral part collides with the inferior glenoid, eventually leading to implant loosening. However, the clinical implications of radiological scapular notching are not fully understood. The percentage of scapular notching after RSA in acute fractures was reported in 11 studies with a median value of 25 [Table 3]. In the study with the longest follow-up 49% of radiographic images were considered abnormal. They reported limited rotation preventing eating, dressing, and body hygiene. Unfortunately, the authors did not report any difference in functional outcome between patients with radiographical scapular notching and patients without such changes. Two systematic reviews have studied the incidence and clinical implications of scapular notching. Nicholson et al.[57] included 24 studies and found that scapular notching appeared between 6 and 14 months postoperatively, with an incidence of 44-96%. Sadoghi et al.[58] included data from five studies and found no correlation between scapular notching and clinical outcome after 24-42 months. At 60 months or more scapular notching was positively correlated with CS pain score and active range of motion. Because of the short follow-up we cannot expect to detect the clinical implications of scapular notching in the vast majority of studies.
Randomized studies with long-term follow-up using the latest techniques of tubercular reinsertion in RSA toward HA are needed. We are in the planning stage of a randomized clinical trial comparing outcome after RSA with HA in complex proximal humeral fractures. It would furthermore be interesting to study possible associations between: (1) The length of follow-up and scapular notching, (2) scapular notching and altered functional outcome, (3) tuberosity fixation techniques and outcome.
 Conclusions Conclusions | |  |
The included clinical studies had a high risk of bias. The level of functional outcome after RSA in acute fractures is so far not clearly superior to HA. However, high complication rates were reported after RSA, and at least 60 months of follow-up seems necessary to study the clinical implications of scapular notching. Based on the available evidence the use of RSA in acute fractures of the proximal humerus is questionable, and we cannot recommend the use of RSA for such fractures outside clinical protocols.
 References References | |  |
| 1. | Bhandari M, Matthys G, McKee MD, Evidence-Based Orthopaedic Trauma Working Group. Four part fractures of the proximal humerus. J Orthop Trauma 2004;18:126-7. 
[PUBMED] |
| 2. | Handoll HH, Ollivere BJ. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev 2012;12:CD000434. 
[PUBMED] |
| 3. | Misra A, Kapur R, Maffulli N. Complex proximal humeral fractures in adults: A systematic review of management. Injury 2001;32:363-72. 
[PUBMED] |
| 4. | Kontakis G, Koutras C, Tosounidis T, Giannoudis P. Early management of proximal humeral fractures with hemiarthroplasty: A systematic review. J Bone Joint Surg Br 2008;90:1407-13. 
[PUBMED] |
| 5. | Boileau P, Krishnan SG, Tinsi L, Walch G, Coste JS, Molé D. Tuberosity malposition and migration: Reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg 2002;11:401-12. 
|
| 6. | George T, Dederichs A, Bellan D, Chaumont PL, Charvet R, Coudane H. Reversed prosthesis for management of complex proximal humeral fractures: a prospective monocenter study. Madrid: 22 nd Congress of SECEC; 2009 [poster]. 
|
| 7. | Grisch D, Riede U, Gerber C, Jost B. Inverse total shoulder arthroplasty as primary treatment for complex proximal humerus fractures in the elderly. Lyon: 23 rd Congress of SECEC; 2011 [poster]. 
|
| 8. | Klein M, Juschka M, Hinkenjann B, Scherger B, Ostermann PA. Treatment of comminuted fractures of the proximal humerus in elderly patients with the Delta III reverse shoulder prosthesis. J Orthop Trauma 2008;22:698-704. 
[PUBMED] |
| 9. | Reuther F, Proust J, Kohut G, Nijs S. Specially designed inverse shoulder prosthesis for the treatment of complex proximal humeral fractures. Lyon: 23 rd Congress of SECEC; 2011 [poster]. 
|
| 10. | Lenarz C, Shishani Y, McCrum C, Nowinski RJ, Edwards TB, Gobezie R. Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res 2011;469:3324-31. 
[PUBMED] |
| 11. | Baulot E, Sirveaux F, Boileau P. Grammont's idea: The story of Paul Grammont's functional surgery concept and the development of the reverse principle. Clin Orthop Relat Res 2011;469:2425-31. 
[PUBMED] |
| 12. | Flatow EL, Harrison AK. A history of reverse total shoulder arthroplasty. Clin Orthop Relat Res 2011;469:2432-9. 
[PUBMED] |
| 13. | Katz D, O›Toole G, Cogswell L, Sauzieres P, Valenti P. A history of reverse shoulder prosthesis. Int J Shoulder Surg 2007;1:108-13. 
 |
| 14. | Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 1993;16:65-8. 
[PUBMED] |
| 15. | Sirveaux F, Navez G, Roche O, Molé D, Williams MD. Reverse prosthesis for proximal humerus fracture, technique and results. Tech Should Surg 2008;9:15-22. 
|
| 16. | Cazeneuve JF, Cristofari DJ. Long term functional outcome following reverse shoulder arthroplasty in the elderly. Orthop Traumatol Surg Res 2011;97:583-9. 
[PUBMED] |
| 17. | Nam D, Kepler CK, Neviaser AS, Jones KJ, Wright TM, Craig EV, et al. Reverse total shoulder arthroplasty: Current concepts, results, and component wear analysis. J Bone Joint Surg Am 2010;92:23-35. 
|
| 18. | Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. J Shoulder Elbow Surg 2011;20:146-57. 
[PUBMED] |
| 19. | Gallinet D, Adam A, Gasse N, Rochet S, Obert L. Interest of the tuberosities reinsertion in complex shoulder fractures treated by reverse prosthesis. Lyon: 23 rd Congress of SECEC; 2011 [abstract]. 
|
| 20. | Levy JC, Badman B. Reverse shoulder prosthesis for acute four-part fracture: Tuberosity fixation using a horseshoe graft. J Orthop Trauma 2011;25:318-24. 
[PUBMED] |
| 21. | Russo R, Cautiero F, Ciccarelli M, Pizzi G, Rotonda GD. The 'Bone Collar-And-Tie' (bCAT) technique: a new solution to restore tuberosity position and cuff tension in reverse shoulder prosthesis for complex proximal humeral fractures. Lyon: 23 rd Congress of SECEC; 2011 [abstract]. 
|
| 22. | Sirveaux F, Navez G, Favard L, Boileau P, Walch G, Mole D. Reverse prosthesis for acute proximal humerus fracture, the multicentric study. In: Walch G, Boileau P, Mole D, Favard L, Levigne C, Sirveaux F, editors. Reverse Shoulder Arthroplasty. Montpellier: Sauramps Médical; 2006. p. 73-80. 
|
| 23. | Sirveaux F, Wein-Remy F, Block D, Sedaghatien J, Roche O, Molé D. Early functional results of the reversed prosthesis for acute fractures in elderly are improved by tuberosity healing. Lyon: 23 rd Congress of SECEC; 2011 [abstract]. 
|
| 24. | Gallinet D, Clappaz P, Garbuio P, Tropet Y, Obert L. Three or four parts complex proximal humerus fractures: Hemiarthroplasty versus reverse prosthesis: A comparative study of 40 cases. Orthop Traumatol Surg Res 2009;95:48-55. 
[PUBMED] |
| 25. | Kontakis G, Tosounidis T, Galanakis I, Megas P. Prosthetic replacement for proximal humeral fractures. Injury 2008;39:1345-58. 
[PUBMED] |
| 26. | Riedel BB, Mildren ME, Jobe CM, Wongworawat MD, Phipatanakul WP. Evaluation of the learning curve for reverse shoulder arthroplasty. Orthopedics 2010;16:237-41. 
|
| 27. | Rockwood CA, Jr. The reverse total shoulder prosthesis. The new kid on the block. J Bone Joint Surg Am 2007;89:233-5. 
|
| 28. | Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: Results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 2006;15:527-40. 
[PUBMED] |
| 29. | Gerber C. Complications and revisions of reverse total shoulder replacements. Nice Shoulder Course 2006:315-7. 
|
| 30. | Cheung E, Willis M, Walker M, Clark R, Frankle MA. Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg 2011;19:439-49. 
[PUBMED] |
| 31. | Farshad M, Gerber C. Reverse total shoulder arthroplasty-from the most to the least common complication. Int Orthop 2010;34:1075-82. 
[PUBMED] |
| 32. | Trappey GJ 4 th , O'Connor DP, Edwards TB. What are the instability and infection rates after reverse shoulder arthroplasty? Clin Orthop Relat Res 2011;469:2505-11. 
|
| 33. | Wierks C, Skolasky RL, Ji JH, McFarland EG. Reverse total shoulder replacement: Intraoperative and early postoperative complications. Clin Orthop Relat Res 2009;467:225-34. 
[PUBMED] |
| 34. | Norris SL, Atkins D. Challenges in using nonrandomized studies in systematic reviews of treatment interventions. Ann Intern Med 2005;142:1112-9. 
[PUBMED] |
| 35. | Audigé L, Bhandari M, Griffin D, Middleton P, Reeves BC. Systematic reviews of nonrandomized clinical studies in the orthopaedic literature. Clin Orthop Relat Res 2004;427:249-57. 
|
| 36. | Deeks JJ, Dinnes J, D'Amico R, Sowden AJ, Sakarovitch C, Song F, et al. Evaluating non-randomized intervention studies. Health Technol Assess 2003;7:iii-x, 1-173. 
|
| 37. | Reitman RD, Kerzhner E. Reverse shoulder arthoplasty as treatment for comminuted proximal humeral fractures in elderly patients. Am J Orthop (Belle Mead NJ) 2011;40:458-61. 
[PUBMED] |
| 38. | Young SW, Segal BS, Turner PC, Poon PC. Comparison of functional outcomes of reverse shoulder arthroplasty versus hemiarthroplasty in the primary treatment of acute proximal humerus fracture. ANZ J Surg 2010;80:789-93. 
[PUBMED] |
| 39. | Dordain F, Emily S, Lebel B, Hulet C, Vielpeau C. The reverse shoulder arthroplasty for proximal humerus fracture patients over 70 years old. Lyon: 23 rd Congress of SECEC; 2011 [poster]. 
|
| 40. | Terragnoli F, Zattoni G, Damiani L, Cabrioli A, Li Bassi G. Treatment of proximal humeral fractures with reverse prostheses in elderly patients. J Orthop Traumatol 2007;8:71-6. 
|
| 41. | Hubert L, Lahogue J-F, Hersan A, Gournay A, Massin P. Reverse Delta prosthesis in shoulder trauma: preliminary results. Rev Chir Orthop Reparatrice Appar Mot 2004;90:116. [Abstract]. 
|
| 42. | Bufquin T, Hersan A, Hubert L, Massin P. Reverse shoulder arthroplasty for the treatment of three-and four-part fractures of the proximal humerus in the elderly: A prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br 2007;89:516-20. 
[PUBMED] |
| 43. | Emily S, Dordain F, Lebel B, Hulet C, Vielpeau C. Influence of restoration of the external rotation in proximal humeral fracture treated with reverse shoulder arthroplasty. Lyon: 23 rd Congress of SECEC; 2011. [Poster]. 
|
| 44. | Sirveaux F, Wein-Remy F, Block D, Sedaghatien J, Mole D. Reverse TSR-does it improve the results in acute fracture arthroplasty? Lyon: 23 rd Congress of SECEC; 2011. [Abstract]. 
|
| 45. | Grisch D, Helmy N, Riede U. Inverse total shoulder arthroplasty as primary treatment for complex proximal humerus fractures in elderly people. Swiss Med Wkly 2010;140:26S. 
|
| 46. | Cazeneuve JF, Cristofari DJ. Grammont reversed prosthesis for acute complex fracture of the proximal humerus in an elderly population with 5-12 years follow-up. Rev Chir Orthop Reparatrice Appar Mot 2006;92:543-8. 
[PUBMED] |
| 47. | Cazeneuve JF, Hassan Y, Kermad F, Brunel A. Delta III reverse-ball-and-socket total shoulder prosthesis for acute complex fractures of the proximal humerus in elderly population. Eur J Orthop Surg Traumatol 2008;18:81-6. 
|
| 48. | Cazeneuve JF. Delta III prosthesis for acute fractures in elderly population with a 1- to 14-year follow-up. J Clin Rehabil Tissue Eng Res 2008;12:10201-4. 
|
| 49. | Cazeneuve JF. Reverse shoulder arthroplasty for acute fractures: retrospective long term outcomes. In: Boileau P, Mole D, Favard L, Levigne C, Sirveaux F, editors. Shoulder Concepts. Montpellier: Sauramps Médical; 2008. p. 163-72. 
|
| 50. | Cazeneuve JF, Cristofari DJ. Delta III reverse shoulder arthroplasty: Radiological outcome for acute complex fractures of the proximal humerus in elderly patients. Orthop Traumatol Surg Res 2009;95:325-9. 
[PUBMED] |
| 51. | Cazeneuve JF, Cristofari DJ. The reverse shoulder prosthesis in the treatment of fractures of the proximal humerus in the elderly. J Bone Joint Surg Br 2010;92:535-9. 
[PUBMED] |
| 52. | Spencer JS, Voloshin I. Reverse shoulder arthroplasty for acute proximal humeral fractures in the geriatric patient: a review of the literature. Geriatr Orthop Surg Rehabil 2011;2:181. 
|
| 53. | den Hartog D, de Haan J, Schep NW, Tuinebreijer WE. Primary shoulder arthroplasty versus conservative treatment for comminuted proximal humeral fractures: A systematic literature review. Open Orthop J 2010;4:87-92. 
[PUBMED] |
| 54. | Poolman RW, Struijs PA, Krips R, Sierevelt IN, Marti RK, Farrokhyar F, et al. Reporting of outcomes in orthopaedic randomized trials: Does blinding of outcome assessors matter? J Bone Joint Surg Am 2007;89:550-8. 
|
| 55. | Hróbjartsson A, Thomsen AS, Emanuelsson F, Tendal B, Hilden J, Boutron I, et al. Observer bias in randomized clinical trials with binary outcomes: Systematic review of trials with both blinded and non-blinded outcome assessors. BMJ 2012;344:e1119. 
|
| 56. | Sirveaux F, Adam A, Gasse N, Rochet S, Obert L. Interest of the tuberosities reinsertion in complex shoulder fractures treated by reversed prosthesis. Lyon: 23 rd Congress of SECEC; 2011. [Abstract]. 
|
| 57. | Nicholson GP, Strauss EJ, Sherman SL. Scapular notching: Recognition and strategies to minimize clinical impact. Clin Orthop Relat Res 2011;469:2521-30. 
[PUBMED] |
| 58. | Sadoghi P, Leithner A, Vavken P, Hölzer A, Hochreiter J, Weber G, et al. Infraglenoidal scapular notching in reverse total shoulder replacement: A prospective series of 60 cases and systematic review of the literature. BMC Musculoskelet Disord 2011;12:101. 
|
[Figure 1]
[Table 1], [Table 2], [Table 3], [Table 4]
| This article has been cited by | | 1 |
Avoiding superior tilt in reverse shoulder arthroplasty: a review of the literature and technical recommendations |
|
| Lior Laver,Grant E. Garrigues | | Journal of Shoulder and Elbow Surgery. 2014; 23(10): 1582 | | [Pubmed] | [DOI] | | | 2 |
Treatment of proximal humeral fractures with reverse shoulder arthroplasty in elderly patients |
|
| C. Iacobellis,A. Berizzi,C. Biz,A. Camporese | | MUSCULOSKELETAL SURGERY. 2014; | | [Pubmed] | [DOI] | | | 3 |
Hospital Readmissions After Surgical Treatment of Proximal Humerus Fractures: Is Arthroplasty Safer Than Open Reduction Internal Fixation? |
|
| Alan L. Zhang,William W. Schairer,Brian T. Feeley | | Clinical Orthopaedics and Related Research®. 2014; | | [Pubmed] | [DOI] | |
|
 |
|
