| |


 |
| Year : 2015 | Volume
: 9
| Issue : 3 | Page : 81-89 |
|
|
|
|
|
ORIGINAL ARTICLE Triple labrum tears repaired with the JuggerKnot™ soft anchor: Technique and results
Vivek Agrawal1, William S Pietrzak2
1 Department of Orthopedics, Marian University School of Medicine; The Shoulder Center, Carmel, IN 46032, USA
2 Department of Bioengineering, University of Illinois at Chicago, Chicago, IL 60607, USA
Correspondence Address:
Vivek Agrawal
The Shoulder Center, 12188A North Meridian Street, Suite 310, Carmel, IN 46032
USA
 Source of Support: Biomet (Warsaw, IN, USA), Conflict of Interest: None
DOI: 10.4103/0973-6042.161440
 |
|
|
|
| Date of Web Publication | 24-Jul-2015 |
 Abstract Abstract | | |
Purpose: The 2-year outcomes of patients undergoing repair of triple labrum tears using an all-suture anchor device were assessed.
Materials and Methods: Eighteen patients (17 male, one female; mean age 36.4 years, range: 14.2-62.3 years) with triple labrum tears underwent arthroscopic repair using the 1.4 mm JuggerKnot Soft Anchor (mean number of anchors 11.5, range: 9-19 anchors). Five patients had prior surgeries performed on their operative shoulder. Patients were followed for a mean of 2.0 years (range: 1.6-3.0 years). Constant-Murley shoulder score (CS) and Flexilevel scale of shoulder function (FLEX-SF) scores were measured, with preoperative and final postoperative mean scores compared with a paired Student's t-test (P < 0.05). Magnetic resonance imaging (MRI) was also performed at final postoperative.
Results: Overall total CS and FLEX-SF scores increased from 52.9 ± 20.4 to 84.3 ± 10.7 (P < 0.0001) and from 29.3 ± 4.7 to 42.0 ± 7.3 (P < 0.0001), respectively. When divided into two groups by whether or not glenohumeral arthrosis was present at the time of surgery (n = 9 each group), significant improvements in CS and FLEX-SF were obtained for both groups (P < 0.0015). There were no intraoperative complications. All patients, including contact athletes, returned to their preinjury level of sports activity and were satisfied. MRI evaluation revealed no instances of subchondral cyst formation or tunnel expansion. Anchor tracts appeared to heal with fibrous tissue, complete bony healing, or combined fibro-osseous healing.
Conclusion: Our results are encouraging, demonstrating a consistent healing of the anchor tunnels through arthroscopic treatment of complex labrum lesions with a completely suture-based implant. It further demonstrates a meaningful improvement in patient outcomes, a predictable return to activity, and a high rate of patient satisfaction.
Level of Evidence: Level IV case series.
Keywords: Labrum tear, multidirectional instability, shoulder arthroscopy, superior labrum anterior and posterior tear, unstable shoulder
How to cite this article:
Agrawal V, Pietrzak WS. Triple labrum tears repaired with the JuggerKnot™ soft anchor: Technique and results. Int J Shoulder Surg 2015;9:81-9 |
 Introduction Introduction | |  |
Soft tissue fixation strength has been shown to be proportional to the number of suture anchors, which when focusing on arthroscopic capsular shift and glenoid labrum repair means stronger repairs require a greater number of fixation points. [1],[2] For shoulder arthroscopy, the suture anchor has become the most commonly utilized method of glenoid labrum fixation. [3],[4] While many factors play a role in the successful treatment of shoulder instability, Boileau et al. in a study focusing on anterior labrum repair, found "the number of sutures and anchors was significantly related to failed arthroscopic stabilization; specifically, patients who had three anchors or fewer had higher rates of recurrent instability (P = 0.03)." [5] Given the limited area available for fixation within the glenoid, increasing the number of suture anchors also introduces additional risks, including osteolysis, failure of fixation, glenoid fracture, and bone loss. [4],[6],[7],[8],[9],[10],[11],[12]
Suture anchors for glenoid fixation have gradually evolved from the original metal-based anchors to bioabsorbable anchors in an effort to avoid possible complications associated with the use of metal anchors. [4],[6] Anchor development has continued to evolve with the introduction of newer composites including polyetheretherketone (PEEK) and calcium ceramics to, hopefully, move toward a better combination of biocompatibility and mechanical stability. [4] Newer anchor designs have pursued fixation differently and are, essentially, all-suture devices. One such anchor is the JuggerKnot Soft Anchor (Biomet, Inc., Warsaw, IN, USA), which is a coreless sleeve and suture construct. Although this device has been studied biomechanically, [13],[14],[15] there have been no prior clinical publications regarding its use. Because triple labrum tears (also referred to as panlabral tears, global labrum tears, and 360° labrum tears in the literature) represent a particularly severe and significant injury requiring extensive labrum repair, we felt this subset of patients would be uniquely suited to evaluate the clinical performance of the 1.4 mm JuggerKnot Soft Anchor. To our knowledge, there are no previously published reports evaluating the clinical performance of an all-suture anchor for triple labrum lesions.
The purpose of this study was to describe the surgical repair techniques and clinical outcomes in a series of patients with triple labrum lesions-combined anterior labrum, posterior labrum, and superior labrum lesions using the anchor. [16],[17],[18],[19] We hypothesize that arthroscopic treatment of complex labrum lesions with the 1.4 mm JuggerKnot Soft Anchor will demonstrate consistent anatomic healing of the anchor tunnels per magnetic resonance imaging (MRI) and a meaningful improvement in clinical outcomes for patients at the 2-year evaluation.
 Materials and Methods Materials and Methods | |  |
As previously described, we divided the glenoid into three distinct zones-the anterior labrum from the 2 o'clock to 6 o'clock positions, the posterior labrum from 6 o'clock to 10 o'clock positions, and the superior labrum from the 10 o'clock to 2 o'clock positions (RIGHT shoulder). [16],[19]
From October 1, 2009 to July 12, 2011, 210 patients had surgical treatment for lesions of the glenoid labrum at our shoulder clinic. 75 of these patients had triple labrum lesions at the time of surgery. All of these patients had a minimum of one suture anchor placed in each of the anterior, posterior, and superior zones, with tears involving at least 270° of the glenoid labrum. 59 of the 70 patients had a labrum pathology treated with the 1.4 mm JuggerKnot Soft Anchor only.
Of the 59 initial qualifying patients, eight patients were covered by workers' compensation insurance and were excluded. Three further patients suffered significant postoperative injuries requiring reoperation and were excluded. Therefore, 48 patients formed the initial eligible pool of patients for the prospective study. The study protocol was fully approved by the Hospital Institutional Review Board, and 26 of the 48 eligible patients enrolled in compliance with the protocol. The 22 patients, who declined participation, did so for a variety of reasons, with the most frequent being the long distance travel that would be required for follow-up. One patient prospectively suffered a significant traumatic injury with confirmed recurrent tear per MRI at approximately 4 months after surgery and was excluded per protocol, as one endpoint of the study protocol was MRI behavior of the anchor tunnel. 18 patients completed the 2-year evaluation per protocol and formed the basis of the present study [Table 1]. Five of the 18 patients had previously had surgery on the same shoulder.
All patients underwent a detailed workup and received appropriate conservative management prior to choosing arthroscopic treatment. Clinical outcomes were assessed using the Constant-Murley Shoulder Score (CS) and the Flexilevel scale of shoulder function (FLEX-SF) preoperatively and at 2-year follow-up. [20],[21],[22],[23] MRI scanning was also performed for all patients at 2-year evaluation to assess the anatomic healing of the suture anchor bone tunnels.
JuggerKnot Soft Anchor description
The JuggerKnot Soft Anchor is a completely suture-based construct made of polyethylene suture (Biomet, Warsaw, IN, USA). The device is supplied with suture passing into and out of a small hole that exists in the wall near each end of the coreless sleeve, allowing both sleeve ends to remain free of the suture. The construct is preloaded onto an inserter. A 1.4 mm diameter hole is drilled into the bone, and the anchor is inserted. When both strands of the MaxBraid suture are tensioned the sleeve bunches, increasing its effective diameter to lock it in the bone hole [Figure 1]. After deployment, the suture remains freely sliding within the sleeve.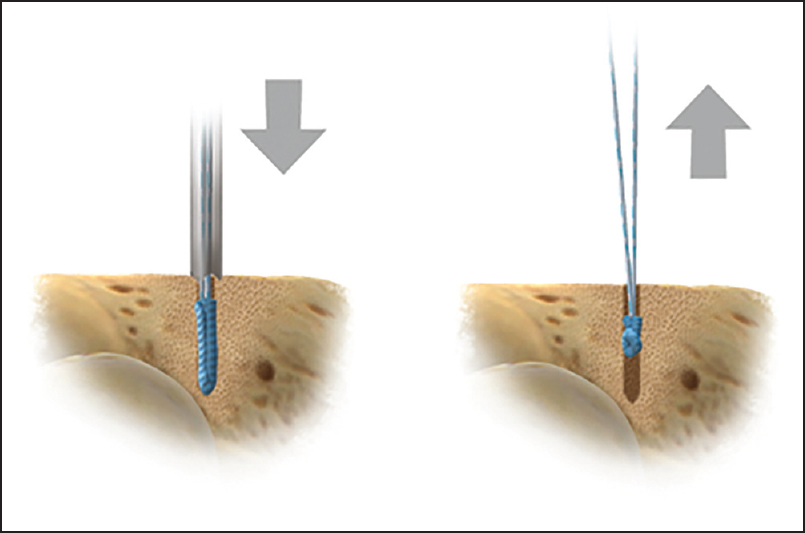 | Figure 1: JuggerKnot Soft Anchor inserted into bone hole (left) and after removal of inserter and tugging on suture legs to set device (right)
Click here to view |
Surgical technique
All patients were placed in the modified lateral decubitus position while awake, and general anesthetic was induced once the patient was fully comfortable in this position. Five to 10 pounds of balanced suspension was used to neutralize the weight of the patient's arm. Several authors have previously detailed the techniques for arthroscopic repair of anterior, posterior, and superior labrum lesions and our approach incorporates previous advances and also includes a few technical points that may be helpful when utilizing an all-suture anchor for labrum repair. [3],[16],[17],[18],[24],[25],[26],[27] For the initial glenohumeral arthroscopy, a low posterolateral portal was utilized that is in line with the lateral border of the acromion and approximately 4 cm inferior to the posterolateral corner of the acromion. [16] Next, an anterolateral portal (8.25 mm twist in cannula) adjacent to the superolateral edge of the subscapularis tendon is established with spinal needle localization for optimal angle of approach to the glenoid. After initial evaluation and any necessary debridement, loose body removal, chondroplasty, and releases the first repair performed when clinically indicated is biceps tenodesis. Our technique is an in situ all-suture technique incorporating the subscapularis tendon and a locking grasping permanent braided suture that maintains the patient's physiologic biceps tendon length. The biceps tendon attachment to the superior labrum is then disconnected.
The superior labrum is then prepared including mobilization of the labrum and light abrasion of the glenoid neck utilizing a full radius shaver. The superior labrum has a significant range of anatomic variability (normal sublabral foramen, Buford complex, absent anterior superior labrum, etc.) and the repair is performed from the posterior superior (10 o'clock RIGHT shoulder) margin with each 1.4 mm anchor placed and tied followed by sequential placement and repair of the labrum more proximally and anteriorly until the superior labrum zone is completed. [25] Gradually work toward the anterolateral cannula in order to minimize the risk of nicking or abrading the previously placed sutures. The anchors are placed with a percutaneous technique with spinal needle localization, minimizing iatrogenic injury to the rotator cuff. The sutures are passed through the labrum via the anterolateral portal using a Spectrum Suture Passer (Conmed Linvatec, Largo, FL, USA) and a solid core shuttle suture [Figure 2]a-d.
The viewing portal is now changed to the superolateral portal for optimal visualization of the inferior glenoid. Along with the anterolateral working portal, an 8.25 mm cannula converts the posterolateral viewing portal to a working portal. The labrum tear is fully mobilized, followed by light abrasion of the glenoid neck utilizing the shaver only. For the repair of the inferior hemisphere zones, place all of the anchors at once utilizing a combination of approaches to optimize the angle of approach to the glenoid face articular margin. Traditional suture anchors that require fixation within the cortical glenoid and perforation, may significantly compromise the mechanical strength of fixation. [28] The JuggerKnot Soft Anchor achieves fixation strength differently and in our experience, cortical perforation and cortical placement of this anchor enhances fixation strength. Therefore, cortical placement of the anchor is preferred when possible. The anchors are placed via the anterolateral cannula, the posterolateral cannula, or the percutaneous spinal needle localization technique. The anchors were approximately placed 5-10 mm apart and an average of 11.5 anchors was used per case (range: 9-19, mode 12). All the suture limbs are retrieved via the anterolateral cannula. Starting at the 6 o'clock position via the posterolateral cannula, the spectrum suture passer is utilized to pass a solid core shuttle suture to achieve anatomic restoration of the capsule-ligamentous complex. A combination of simple and horizontal mattress sutures is utilized to help restore the labral height and achieve a more uniform rounded bumper cushion. [29],[30] Each suture is placed and tied, and the sequence is repeated in the posterior and anterior zones until the entire repair is completed. Typically, we complete the posterior inferior zone and a portion of the anterior inferior zone via the posterolateral cannula before retrieving the remaining anterior zone sutures via the posterolateral cannula and completing the anterior zone repair from the anterolateral cannula. After completing the repair and any additional indicated capsular plication, balanced tension in the entire capsule-ligamentous complex combined with a full range of motion and a centralized humeral head is confirmed [Figure 3]a-d. Any remaining indicated procedures were subsequently performed [Table 2]. Following routine closure of the portals with simple sutures, the patient was placed in an abductor pillow immobilizer (Shoulder Abduction Pillow, BREG, Vista CA, USA).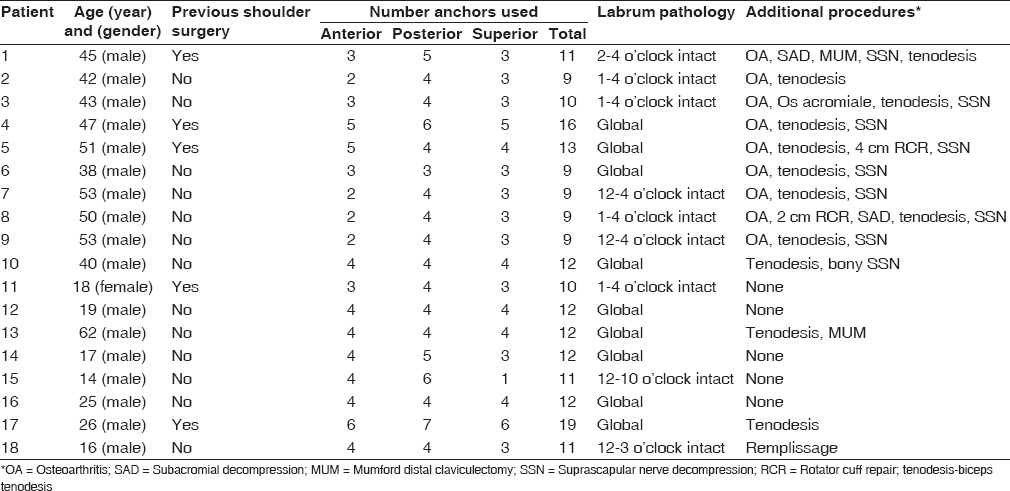 | Table 2: Details of anchor quantities used, labrum pathology, and additional procedures performed
Click here to view |
Postoperative rehabilitation
All patients participated in the same postoperative rehabilitation program. The abduction pillow was worn full time except for hand and elbow range-of-motion, and pendulum exercise 1-month following surgery. After the abduction pillow had been discontinued, supine passive and active assisted exercises were initiated to restore range of motion at 1-month following surgery. Patients were advised not to try and actively lift the arm when upright until 3 months after surgery. Active supine range of motion exercises was started at 8 weeks following surgery, along with gradual muscle and functional strengthening exercises 12 weeks following surgery. Sports and activity specific rehabilitation was initiated once appropriate scapular control baseline strength was achieved. Thereafter, activities were increased gradually with a return to heavy manual labor and contact sports delayed until at least 6 months following surgery.
Validated shoulder outcome scores were assessed in person using the CS and the FLEX-SF at 2-year follow-up.
Statistical analysis
Comparisons were made between preoperative and 2-year postoperative outcome scores. All comparisons were analyzed with the use of a paired Student's t-test, with an alpha of 0.05 established for significance.
Imaging
All patients at the 2-year follow-up had an MRI utilizing a 1.5 Tesla high-field scanner (Signa; GE Medical Systems, Milwaukee, WI, USA). Gradient-echo axial, proton density and T2-weighted oblique coronal and sagittal, and coronal fat-suppressed imaging of the shoulder were performed utilizing a dedicated shoulder coil. Sagittal T1-weighted series were also obtained. Two musculoskeletal fellowship-trained radiologists, who were aware that the patients had undergone surgery for shoulder instability but were blinded to the specific details of each patient's repair, reviewed the images. Blinding was instituted to minimize the potential for bias during radiological evaluation.
 Results Results | |  |
Operative procedures in addition to labrum pathology repair and anchor number and placement are presented in [Table 2]. Nine patients had global circumferential detachment of the labrum, and the other nine patients had one area of labrum intact or absent (normal sublabral foramen, Buford complex, etc.). Five patients had previous surgery on the same shoulder. The outcomes for the 18 shoulders were assessed after a mean duration of follow-up of 2-year (1.6-3.0 years). Outcome measures, including the preoperative and the most recent Constant and FLEX-SF scores, are summarized in [Table 3]. Overall, mean total constant score increased from 52.9 to 84.3 (P < 0.0001) and mean FLEX-SF score increased from 29.3 to 42.0 (P < 0.0001). There were no intraoperative complications. All 18 shoulders had improvement when the postoperative scores were compared with the preoperative scores. At the final clinical follow-up evaluation all patients, including contact athletes, had been able to resume their preinjury level of sports activity, were satisfied with the results and would elect to have the procedure again. One patient dislocated the other shoulder 3 years following surgical repair during a playoff football game and at surgery had a similar pattern of labrum tearing to the other side.
All patients at the 2-year follow-up had an MRI utilizing a 1.5 Tesla high-field scanner (Signa; GE Medical Systems, Milwaukee, WI, USA). As an added benefit for postoperative evaluation, the all-suture JuggerKnot Soft Anchor did not hinder diagnostic imaging. There were no instances of subchondral cyst formation or tunnel expansion. The suture anchor tracts appeared to heal with fibrous tissue, complete bony healing, or some combined fibro-osseous healing of the tunnels [Figure 3]a-d. There was evidence of each type of healing among the multiple suture anchor tracts present in each patient.
One of the revision patients was a competitive swimmer that was initially treated for a global labrum tear at our shoulder clinic and tripped and fell down stairs in the early postoperative course requiring revision global labrum repair. Despite having multiple anchors adjacent to each other, for this patient along with the others, no evidence of tunnel expansion was evident.
 Discussion Discussion | |  |
Arthroscopic management of shoulder instability has evolved greatly and rather than a unilateral approach to shoulder instability evaluation and treatment, the circle concept of shoulder instability described by Warren predicts that pathology can exist in multiple zones concurrently and successful treatment requires appropriate evaluation and treatment in all zones to restore balanced function. [31],[32],[33],[34] Combined lesions of the glenoid labrum involving tears of the anterior, posterior, and superior labrum are relatively rare, and only a few studies have reported on the outcomes of treatment in these patients. [16],[18],[19],[24] Detecting these lesions preoperatively and distinguishing them from unidirectional labral tears can be difficult, and successful treatment requires a high index of suspicion and the ability to evaluate and treat pathology in all areas. [19],[35]
The JuggerKnot anchor was designed as an all-suture construct to avoid potential sequalae from the migration and third body wear of a rigid anchor body, to provide radiographic images unobscured by metal hardware, and to facilitate revision procedures. The small 1.4 mm diameter of the drill hole helps to minimize compromise to the bone while allowing for multiple points of soft tissue fixation. While several published studies have compared the biomechanical properties of the JuggerKnot anchor with other types of suture anchors, [16],[17],[18] this is the first published clinical study of this device.
Lo and Burkhart evaluated seven patients with a mean age of 25 years (range: 17-36 years) with two of the seven patients having a global labrum lesion. The median number of anchors (3.0-mm BioFastak, Arthrex, Naples, FL, USA) used for labral repair was seven (range: 5-9 anchors). Six of seven patients were satisfied with the procedure at a mean of 12.7 months (range: 6-43 months) with one subsequently having a shoulder hemiarthroplasty. [16]
Tokish et al. studied 41 shoulders in 39 patients in a military population with a mean age of 25.1 years (range: 17-38 years) with global labrum lesions from multiple treating centers. They repaired the labrum circumferentially with 3.0-mm Bio-SutureTak (Arthrex, Naples, FL, USA) absorbable or PEEK anchors (Arthrex, Naples, FL, USA) with #2 FiberWire (Arthrex, Naples, FL, USA), with a mean of 7.1 (range not reported) suture anchors. Follow-up was performed at a mean of 31.8 months (range: 24-53 months). Six shoulders required revision surgery and one further patient, a wrestler, retired from competition after two seasons citing the shoulder as a contributing factor. [24] Mean preoperative and postoperative modified American Shoulder and Elbow Surgeon scores (ASES), short form-12 scores (SF-12), and single assessment numeric evaluation score were 55.5 and 89.6, 75.7, and 90.9, and 36.7 and 88.5, respectively (P < 0.01 for all).
Ricchetti et al. retrospectively studied 44 patients with a mean age of 32 years (range: 15-55 years) with several treating surgeons. [19] The number and type of anchors used were at the discretion of the treating surgeon and anchor sizes included 2.4 mm (Bio-SutureTak), 2.9 mm PushLock (Arthrex, Naples, FL, USA), and 3.0 mm (Bio-SutureTak). The mean number of anchors per repair was 7.9 (range: 5-12), with a mean of 3.3 anchors (range: 1-5) used anteriorly, 2.4 (range: 1-6) used posteriorly, and 2.4 (range: 1-3) used superiorly. At final follow-up (mean 42 months, range: 16-78 months), 69% of patients stated that they had returned to their preinjury level of function. 13 complications (30%) developed in the postoperative period, with 3 (7%) requiring a second surgery. One patient developed symptomatic glenohumeral arthritis 3 years after surgery and underwent total shoulder arthroplasty 4 years after repair. Mean postoperative ASES score and Penn Shoulder score were 90.1 and 90.2, respectively.
In comparison to these prior reports, our current series of patients represents a more diverse general population with an older mean age 36.4 years (range: 14.2-62.3 years). The patients in this group represent two further subgroups-the more acutely symptomatic patient that sustained a traumatic injury with persistent and recurrent symptoms of both pain and instability and the more chronically symptomatic patient that may have had a remote injury that with time and progression of symptoms presented with more primary complaints of shoulder pain rather than instability and findings consistent with a combination of persistent shoulder instability and developing glenohumeral arthrosis. The patients [9 of 18, patients 1-9, [Table 2]] with glenohumeral arthrosis at the time of surgical treatment had a mean age of 46.9 years (range: 38-53 years), while the other nine patients [patients 10-18, [Table 2]] had a mean age of 26.3 years (range: 14-62 years). Consistent with the findings of the other studies, both groups of patients were satisfied with the procedure and obtained meaningful and statistically significant improvement in clinical outcomes (mean Constant score improvements of 31 points/P = 0.0014 and 32 points/P = 0.0015, respectively; and mean SF-12 score improvements of 10 points/P = 0.0031 and 15 points/P < 0.001, respectively). In contrast to the anchors used in the other studies, the 1.4 mm JuggerKnot Soft Anchor is much smaller and is loaded with a single #1 MaxBraid Suture allowing the anchors to be placed in closer proximity to achieve a greater number of fixation points within a similar area. The average number of total anchors in our study was 11.5 (range: 9-19) with a mean 3.6 anchors in the anterior zone (range: 2-6), 4.4 anchors in the posterior zone (range:3-7), and 3.4 anchors in the superior zone (range: 1-6).
In addition to validated clinical outcomes, anatomic behavior of the anchor tunnels was also studied utilizing MRI. There were no instances of subchondral cyst formation or tunnel expansion. The suture anchor tunnels appeared to heal with fibrous tissue, complete bony healing, or some combined fibro-osseous healing of the tunnels [Figure 4]a-d. The suture anchor tunnels appeared to heal with fibrous tissue, complete bony healing, or some combined fibro-osseous healing [Figure 4]a-d, with representation of each type of healing present in each patient. We suspect that these phases may represent the natural progression of healing of the tunnels, but repeat imaging at longer follow-up would be required to confirm this. While these preliminary results are encouraging, we echo the sentiments of Tokish et al. "It is unclear whether instability rates will increase over time or if there will be detrimental effects in association with the placement of a mean of 7.1 suture anchors in the shoulder." [24]
This study had several limitations. Because our study did not use a comparison group, such as patients treated nonoperatively or with an alternative treatment technique, the clinical outcomes cannot be directly compared with alternative forms of treatment. The current study is also limited to a relatively short follow-up and as one patient in two of the three prior studies developed significant arthrosis requiring conversion to a shoulder replacement, only longer follow-up will clarify whether these patients are at an increased risk of developing arthrosis beyond the already known risk of arthrosis with persistent shoulder instability. Nine of the patients in the present study already had significant arthrosis and were treated for improvement in current pain and function, and it remains to be seen whether significant symptomatic progression of their arthrosis will develop over time. [16],[19],[24]
 Conclusion Conclusion | |  |
To our knowledge, this is the first study to prospectively study the clinical and MRI outcomes of patients with triple labral lesions arthroscopically treated with a completely suture-based implant. Our results are encouraging, demonstrating a consistent healing of the anchor tunnels through arthroscopic treatment of complex labrum lesions with a completely suture-based implant. It further demonstrates a meaningful improvement in patient outcomes, a predictable return to activity, and a high rate of patient satisfaction.
 References References | |  |
| 1. | Jost PW, Khair MM, Chen DX, Wright TM, Kelly AM, Rodeo SA. Suture number determines strength of rotator cuff repair. J Bone Joint Surg Am 2012;94:e100.  |
| 2. | Black KP, Schneider DJ, Yu JR, Jacobs CR. Biomechanics of the Bankart repair: The relationship between glenohumeral translation and labral fixation site. Am J Sports Med 1999;27:339-44.  |
| 3. | Wolf EM, Wilk RM, Richmond JC. Arthroscopic Bankart repair using suture anchors. Oper Tech Orthop 1991;1:184-91.  |
| 4. | Dhawan A, Ghodadra N, Karas V, Salata MJ, Cole BJ. Complications of bioabsorbable suture anchors in the shoulder. Am J Sports Med 2012;40:1424-30.  |
| 5. | Boileau P, Villalba M, Héry JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 2006;88:1755-63.  |
| 6. | Kaar TK, Schenck RC Jr, Wirth MA, Rockwood CA Jr. Complications of metallic suture anchors in shoulder surgery: A report of 8 cases. Arthroscopy 2001;17:31-7.  |
| 7. | Steinmann SP. Cause of glenoid rim fracture. Arthroscopy 2009;25:1061-2.  [ PUBMED] |
| 8. | Spoliti M. Glenoid osteolysis after arthroscopic labrum repair with a bioabsorbable suture anchor. Acta Orthop Belg 2007;73:107-10.  |
| 9. | Park MJ, Hsu JE, Harper C, Sennett BJ, Huffman GR. Poly-L/D-lactic acid anchors are associated with reoperation and failure of SLAP repairs. Arthroscopy 2011;27:1335-40.  |
| 10. | Fritsch BA, Arciero RA, Taylor DC. Glenoid rim fracture after anchor repair: A report of 4 cases. Am J Sports Med 2010;38:1682-6.  |
| 11. | Banerjee S, Weiser L, Connell D, Wallace AL. Glenoid rim fracture in contact athletes with absorbable suture anchor reconstruction. Arthroscopy 2009;25:560-2.  |
| 12. | Park HB, Keyurapan E, Gill HS, Selhi HS, McFarland EG. Suture anchors and tacks for shoulder surgery, part II: The prevention and treatment of complications. Am J Sports Med 2006;34:136-44.  |
| 13. | Barber FA, Herbert MA, Hapa O, Rapley JH, Barber CA, Bynum JA, et al. Biomechanical analysis of pullout strengths of rotator cuff and glenoid anchors:2011 update. Arthroscopy 2011;27:895-905.  |
| 14. | Mazzocca AD, Chowaniec D, Cote MP, Fierra J, Apostolakos J, Nowak M, et al. Biomechanical evaluation of classic solid and novel all-soft suture anchors for glenoid labral repair. Arthroscopy 2012;28:642-8.  |
| 15. | Barber FA, Herbert MA. Cyclic loading biomechanical analysis of the pullout strengths of rotator cuff and glenoid anchors: 2013 update. Arthroscopy 2013;29:832-44.  |
| 16. | Lo IK, Burkhart SS. Triple labral lesions: Pathology and surgical repair technique-report of seven cases. Arthroscopy 2005;21:186-93.  |
| 17. | Seroyer ST, Nho SJ, Provencher MT, Romeo AA. Four-quadrant approach to capsulolabral repair: An arthroscopic road map to the glenoid. Arthroscopy 2010;26:555-62.  |
| 18. | Tokish JM, McBratney CM, Solomon DJ, Leclere L, Dewing CB, Provencher MT. Arthroscopic repair of circumferential lesions of the glenoid labrum: surgical technique. J Bone Joint Surg Am 2010; 92 Suppl 1 Pt 2:130-44. doi: 10.2106/JBJS.J.00234.  |
| 19. | Ricchetti ET, Ciccotti MC, O′Brien DF, DiPaola MJ, DeLuca PF, Ciccotti MG, et al. Outcomes of arthroscopic repair of panlabral tears of the glenohumeral joint. Am J Sports Med 2012;40:2561-8.  |
| 20. | Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Related Res 1987;214:160-4.  |
| 21. | Cook KF, Monahan PO, McHorney CA. Delicate balance between theory and practice: Health status assessment and item response theory. Med Care 2003;41:571-4.  [ PUBMED] |
| 22. | Cook KF, Roddey TS, Gartsman GM, Olson SL. Development and psychometric evaluation of the Flexilevel Scale of Shoulder Function. Med Care 2003;41:823-35.  |
| 23. | Cook KF, Roddey TS, O′Malley KJ, Gartsman GM. Development of a Flexilevel Scale for use with computer-adaptive testing for assessing shoulder function. J Shoulder Elbow Surg 2005;14 1 Suppl S:90S-4.  |
| 24. | Tokish JM, McBratney CM, Solomon DJ, Leclere L, Dewing CB, Provencher MT. Arthroscopic repair of circumferential lesions of the glenoid labrum. J Bone Joint Surg Am 2009;91:2795-802.  |
| 25. | Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg 1995;4:243-8.  |
| 26. | Goubier JN, Iserin A, Duranthon LD, Vandenbussche E, Augereau B. A 4-portal arthroscopic stabilization in posterior shoulder instability. J Shoulder Elbow Surg 2003;12:337-41.  |
| 27. | Paxton ES, Backus J, Keener J, Brophy RH. Shoulder arthroscopy: Basic principles of positioning, anesthesia, and portal anatomy. J Am Acad Orthop Surg 2013;21:332-42.  |
| 28. | Lim TK, Koh KH, Lee SH, Shon MS, Bae TS, Park WH, et al. Inferior anchor cortical perforation with arthroscopic Bankart repair: A cadaveric study. Arthroscopy 2013;29:31-6.  |
| 29. | Slabaugh MA, Friel NA, Wang VM, Cole BJ. Restoring the labral height for treatment of Bankart lesions: A comparison of suture anchor constructs. Arthroscopy 2010; 26:587-91.  |
| 30. | Hagstrom LS, Marzo JM. Simple versus horizontal suture anchor repair of Bankart lesions: Which better restores labral anatomy? Arthroscopy 2013;29:325-9.  |
| 31. | Warren RF. Subluxation of the shoulder in athletes. Clin Sports Med 1983;2:339-54.  |
| 32. | Altchek DW, Skyhar MJ, Warren RF. Shoulder arthroscopy for shoulder instability. Instr Course Lect 1989;38:187-98.  [ PUBMED] |
| 33. | Curl LA, Warren RF. Glenohumeral joint stability. Selective cutting studies on the static capsular restrains. Clin Orthop Relat Res 1996;330:54-65.  |
| 34. | O′Brien SJ, Neves MC, Arnoczky SP, Rozbruck SR, Dicarlo EF, Warren RF, et al. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med 1990;18:449-56.  |
| 35. | Lindauer KR, Major NM, Rougier-Chapman DP, Helms CA. MR imaging appearance of 180-360 degrees labral tears of the shoulder. Skeletal Radiol 2005;34:74-9.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
[Table 1], [Table 2], [Table 3]
|
