| |


 |
| Year : 2015 | Volume
: 9
| Issue : 3 | Page : 94-98 |
|
|
|
|
|
CASE REPORT One step arthroscopically assisted Latarjet and posterior bone-block, for recurrent posterior instability and anterior traumatic dislocation
Riccardo D'Ambrosi1, Carlo Perfetti2, Guido Garavaglia3, Ettore Taverna4
1 Department of Shoulder Surgery, IRCCS Galeazzi Orthopaedic Institute, Milan,
2 Department of Shoulder Surgery, IRCCS Galeazzi Orthopaedic Institute, Milan, Italy,
3 Department of Surgery, Upper Limb Unit, OBV, Mendrisio, Switzerland,
4 Department of Shoulder Surgery, IRCCS Galeazzi Orthopaedic Institute, Milan, Italy; Department of Surgery, Upper Limb Unit, OBV, Mendrisio, Switzerland,
Correspondence Address:
Riccardo D'Ambrosi
Department of Shoulder Surgery, Istituto Ortopedico Galeazzi, Milan, Italy
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.161449
 |
|
|
|
| Date of Web Publication | 24-Jul-2015 |
 Abstract Abstract | | |
This case presents the challenges of the surgical management for a patient with a history of recurrent posterior shoulder instability and subsequently traumatic anterior dislocation. The patient was already on the waiting list for an arthroscopic posterior stabilization with anchors, when a car accident caused an additional anterior shoulder dislocation. This traumatic anterior dislocation created a bone loss with a glenoid fracture and aggravated the preexisting posterior instability. In order to address both problems, we decided to perform an arthroscopically assisted Latarjet procedure for anterior instability and to stabilize with a bone graft for posterior instability. To our best knowledge, this type of surgical procedure has so far never been reported in the literature. The purpose of this report is to present the surgical technique and to outline the decision making process.
Keywords: Arthroscopically assisted Latarjet, bone-block, glenoid bone loss, multidirectional instability
How to cite this article:
D'Ambrosi R, Perfetti C, Garavaglia G, Taverna E. One step arthroscopically assisted Latarjet and posterior bone-block, for recurrent posterior instability and anterior traumatic dislocation. Int J Shoulder Surg 2015;9:94-8 |
How to cite this URL:
D'Ambrosi R, Perfetti C, Garavaglia G, Taverna E. One step arthroscopically assisted Latarjet and posterior bone-block, for recurrent posterior instability and anterior traumatic dislocation. Int J Shoulder Surg [serial online] 2015 [cited 2016 Sep 20];9:94-8. Available from: http://www.internationalshoulderjournal.org/text.asp?2015/9/3/94/161449 |
 Introduction Introduction | |  |
Surgical intervention for shoulder instability should be considered in patients who continue to experience debilitating symptoms despite completion of an appropriate rehabilitation regimen [Table 1].
Surgical management should be individualized to address the anatomic cause of shoulder instability. The ratio of our technique is to reconstruct, in the most anatomically way possible, the glenoid of the patient in view of the young age and the associated hyperlaxity. The purpose of this case report is to illustrate the history of a young man with recurrent posterior dislocation of the shoulder caused by joint laxity associated with a high-energy trauma that caused anterior dislocation with bone loss and subsequent instability.
 Case report Case report | |  |
A 23-year-old male was sent to our institution. The patient had a 3 years history of shoulder pain and sense of posterior instability with recurrent episodes of posterior subluxation events. He experienced had many of these episodes during normal activity of daily living.
Nonsurgical approach did not lead to any benefit. During the first consultation, the patient had a full range of motion, demonstrable generalized ligamentous laxity, hyperextension at the elbows and wrists. All impingement tests were negative, and all strength tests equally. There was a 1.8 cm sulcus sign on the left shoulder, as well as a positive apprehension sign. He demonstrated loss of external rotation of approximately 12° on his left extremity, as compared to his right extremity.
In the light of the imaging and clinical presentation, we diagnosed a recurrent posterior instability. We suggested to perform an arthroscopic posterior capsulo-labral repair and surgery was scheduled.
While waiting for surgery the patient had a car accident and sustained a traumatic anterior dislocation of the left shoulder. The dislocation was reduced in the emergency room, and physical treatment started after 1 week [Figure 1]. A new visit was scheduled 4 weeks after the car accident and the patient reported a worsening of instability with extreme apprehension and several new episodes of dislocation which he to be both anterior and posterior and that he was able to reduce by himself.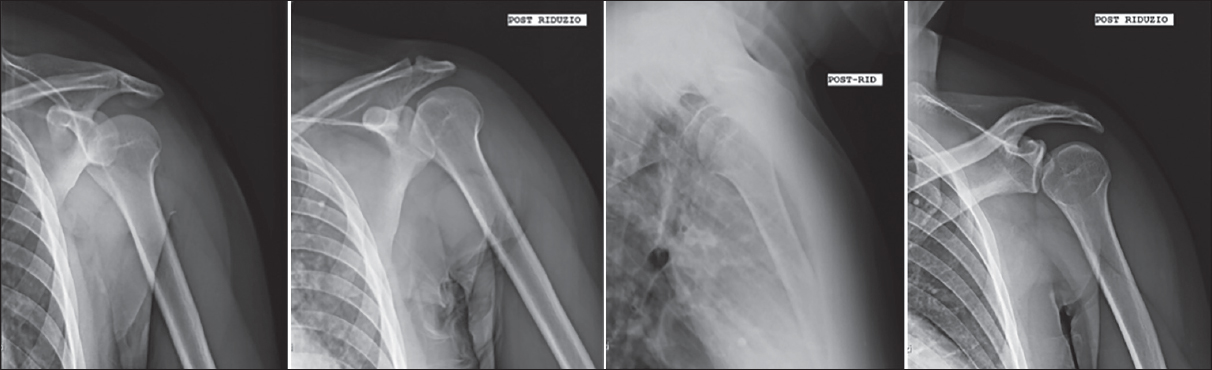 | Figure 1: Rx left shoulder: In the first image dislocated shoulder immediately after the trauma. In subsequent images: Rx control of the left sholder after reduction.
Click here to view |
At physical examination his range of motion was 110° of flexion, extrarotation 15°, intrarotation arrived to L-5. Tests for rotator cuff were negative, but the patient had a loss of strength. Tests for instability were all positive (sulcus, Rowe and load and shift test). No vascular or nervous impairment were present.
For further evaluation we performed a computed tomography scan that revealed a Hill-Sachs lesion at the posterior aspect of the humeral head, 10-15% (of the total glenoid surface) bone loss at the anterior glenoid rim and about 10% bone posteriorly [Figure 2].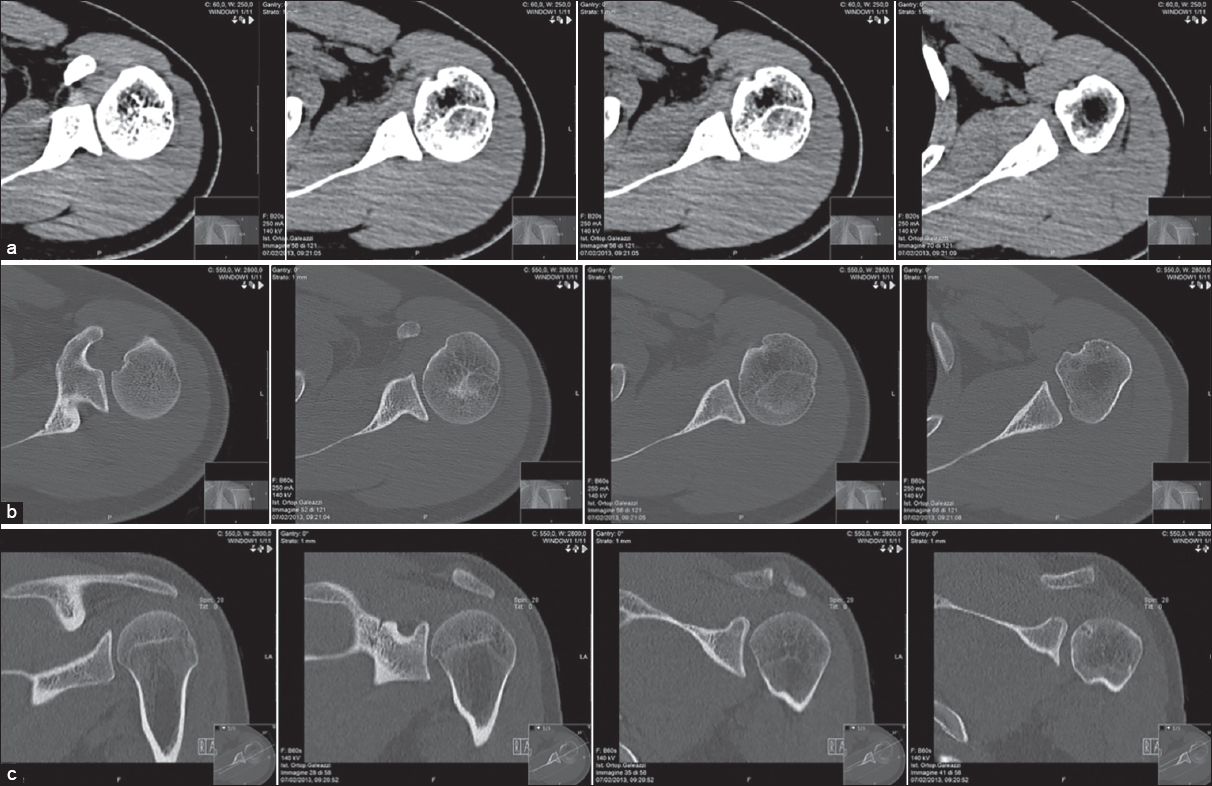 | Figure 2: Pre-operative computed tomography images. Axial and sagittal view. Left shoulder: humeral head that presents focal cortical erosion with small subcortical cystic-dystrophic irregularities along the anterior superior medial side. Incision of the profi le cortex of the humeral head on the rear side. (a-b) Axial view (c) sagittal view
Click here to view |
After careful assessment of the new situation, we decided to treat both instability and associated osseous defects, with a combined arthroscopically assisted Latarjet procedure and posterior bone-block.
Surgical technique
The patient was placed in the beach chair position. The draping gave access to the posterior and anterior aspects of the shoulder girdle and allowed the arm to be mobilized intra-operatively. A high posterior lateral view portal was preferred for initial glenohumeral inspection so as to allow a drill guide to be inserted posteriorly into the joint. Standard anterior, superior and mid-glenoid portals were made by means of 5.5 mm and 7.0 mm cannulas.
At joint inspection, we confirmed that the glenoid bone defects were present both anteriorly and posteriorly, with a deficient anterior capsulo-labral complex. The remaining anterior labrum and capsule were detached from the anterior rim of the glenoid by combining an elevator, a shaver, and a radio frequency device. The capsulo-labral complex was freed to view the subscapularis muscle fibers. The anterior bony glenoid defect was then smoothed and freshened with a motorized bur [Figure 3].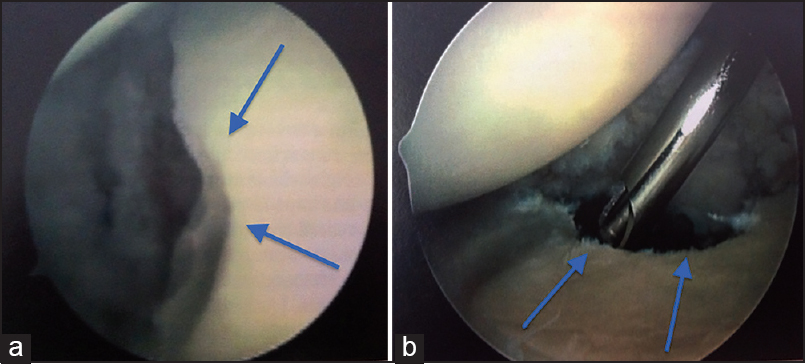 | Figure 3: Arthroscopic view of the glenoid bone defect. (a) Anterior portal (b) posterior portal
Click here to view |
We also used a special drill guide that allowed us to place two drill sleeves, parallel to the glenoid face and to one another as well, perpendicularly around the glenoid neck [Figure 4] and [Figure 5]. Furthermore we removed the scope and the cannulas and proceeded with the open part of the procedure.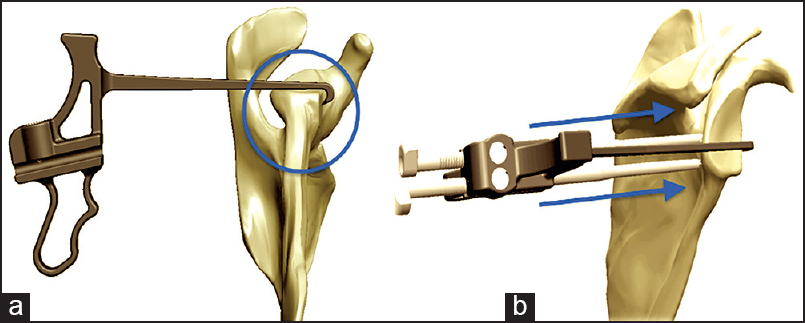 | Figure 5: (a)The guide is rotated to capture the anterior edge of the glenoid under the hook. The hook should be placed at the 4 o'clock position which will correlate with the mid point of the coracoid. The Glenoid Guide should also align with the placement of the spinal needle. (b) Once the hook is positioned, a bullet is placed in the superior hole of the guide. A small skin incision is made and the bullet is advanced until it firmly contacts the posterior aspect of the glenoid neck. The ratchet teeth of the bullet should be aligned with the screws adjacent to the handle of the guide. The process is repeated for the inferior bullet.
Click here to view |
Arthrotomy was then executed by means of a limited deltopectoral approach, incorporating the mid glenoid portal at the top of the incision. After having executed the coracoid osteotomy, we removed the soft tissue and a layer of cortical bone with the saw. Thus, the inferior surface was prepared and created a flat surface of bleeding bone. At this point, a single drill hole was made within 5 mm of the apex in the central axis of the coracoid. A subscapularis split was operated at the junction between the superior two-thirds and the inferior one-third. In this way the previously prepared capsulo-labral complex was identified, and the glenoid was exposed by using a Fukuda retractor and two Hohmann retractors. A flexible guide wire was then put, from the back to the front, in the superior drill sleeve and passed through the superior coracoid hole. Next we passed the coracoid and the conjoint tendon through the subscapularis split and placed the graft with the freshened surface in front of the glenoid neck. A 34 mm partially threaded cannulated screw was then placed through the superior coracoid hole after having removed the superior sleeve. All of this by means of the flexible guide wire. The inferior coracoid hole was then drilled from the posterior part through the drill sleeve. The inferior sleeve was then also removed and a second cannulated partially threaded 34 mm screw was placed over the guide wire.
By means of the wires that were passing through the sleeves, we were able to attach the coracoid flush to the glenoid, compressed by two screws, perfectly parallel one to another and both perpendicular to the glenoid neck. In this way, the coracoid and the conjoined tendon remained as extra-articular stabilizers.
The second step concerned the incision in the left iliac crest. The incision of the skin and the subcutaneous tissue was necessary to be able to reach the bone segment. We proceeded to the removal of the fragment of about 2 cm long by 1 cm wide. Hemostasis suture.
With regard to the third step, we engraved the back of the shoulder by means of a blunt dissection to reach the deltoid. We ran split of the deltoid muscle and reached the infraspinatus muscle. We split the infraspinatus. Capsulotomy. We reached the posterior margin of the scapula. We shaved the posterior margin and placed the bone graft with a malleolar screw of 34 mm. We implanted the placement [Table 2]. Hemostasis suture. Medication and tutor [Figure 6] and [Figure 7]. 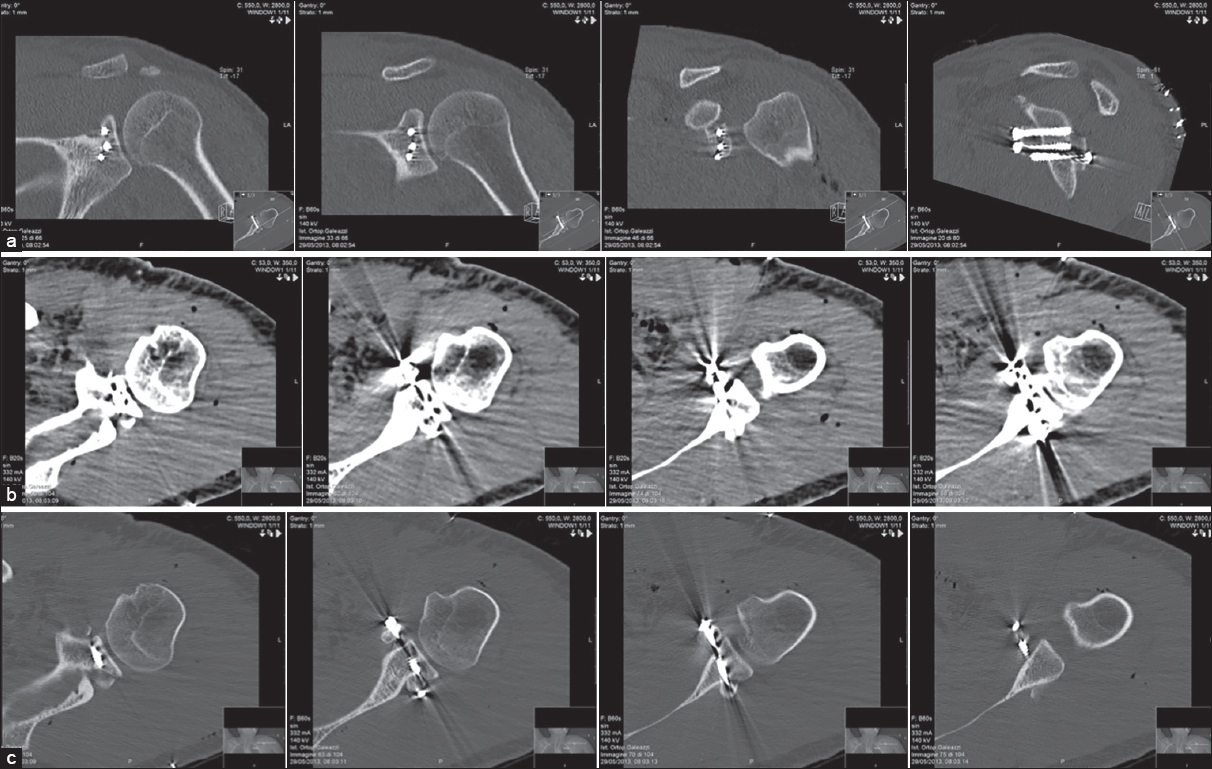 | Figure 6: Post-operative computed tomography images, left shoulder showing. shoulder stabilization with coracoid transposition fixed with two screws at the front edge of the glenoid; posteriorly with a screw and bone graft (removal of the iliac crest) along the posterior margin of the glenoid.(a-b) Axial view (c) sagittal view
Click here to view |
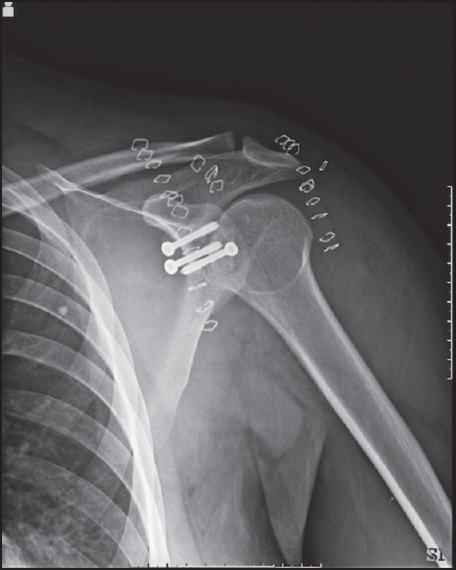 | Figure 7: Antero-posterior Rx image, left shoulder. Day after surgery. Correct anterior coracoid and posterior bone graft positioning
Click here to view |
Postoperative rehabilitation
The arm was placed in a standard protective sling for 3 weeks, but passive- and active-assisted range of motion exercises had begun immediately after the discharge, which is usually at day 2 or 3. External rotation was limited to 30° during the 1 st month and strengthening exercises started.
Clinical result
The postoperative course was uneventful. The shoulder was immobilized in a sling for 3 weeks, but scapular control and core work were begun immediately. As of the 4 th week, a full rehabilitation program was started.
At 1 year after surgery the patient is fully satisfied. There were no episodes of dislocation. The range of motion is full (Flexion 180°, Abduction 180°, External rotation 70°, Internal rotation 100°) and pain is gradually decreasing (maximum VAS 5). The patient also has resumed his normal occupation (postman).
 Discussion Discussion | |  |
The Latarjet procedure is the gold standard for the treatment for chronic anterior instability in patients with large bone defects. [1]
Arthroscopic Latarjet has been described for the 1 st time by Lafosse. [2]
We decided to perform an arthroscopically assisted Latarjet because the placement of the bone graft is more accurate under arthroscopic control, several different views can be afforded by the arthroscopic technique that improve graft placement and reduce the chances of overhang and impingement; concurrent anterior and posterior instability can be treated during the same arthroscopic surgical procedure using anterior and posterior bone blocks, this is not possible through a single open approach; even though the strength of the bone-block fixation allows early mobilization, the risk of adhesions and shoulder stiffness is higher with an open technique than with arthroscopy; if during an intended Bankart repair the tissue is determined to not be reconstructable, then an arthroscopic Latarjet offers an alternative to traditional open surgery without potentially having to reposition the patient.
Concerning posterior instability several procedures have been proposed. Many authors [3],[4] have reported excellent results in the literature regarding the treatment of the instability with posterior bone block. Hence, we decided to associate with Latarjet.
The result with our case seems encouraging with no recurrent instability (posterior or anterior) reported at 1 year. The simultaneous arthroscopically assisted Latarjet and posterior bone-block has not been described yet. This type of surgery can provide several advantages for the treatment of multidirectional instability with bone loss, but must be performed only by expert surgeons.
 Conclusions Conclusions | |  |
This is a case that has never been described in the literature before. Undoubtedly, to evaluate the long-term results and the effectiveness of the result we would need a greater sample of patients. One alone is not indicative, over that of a longer follow-up. In our experience, however, we can state the case as described above currently represents an excellent alternative in cases of traumatic anterior and posterior recurrent dislocation.
 References References | |  |
| 1. | Cerciello S, Edwards TB, Walch G. Chronic anterior glenohumeral instability in soccer players: Results for a series of 28 shoulders treated with the Latarjet procedure. J Orthop Traumatol 2012;13:197-202.  |
| 2. | Lafosse L, Lejeune E, Bouchard A, Kakuda C, Gobezie R, Kochhar T. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy 2007;23:1242.e1-5.  |
| 3. | Barbier O, Ollat D, Marchaland JP, Versier G. Iliac bone-block autograft for posterior shoulder instability. Orthop Traumatol Surg Res 2009;95:100-7.  |
| 4. | Servien E, Walch G, Cortes ZE, Edwards TB, O′Connor DP. Posterior bone block procedure for posterior shoulder instability. Knee Surg Sports Traumatol Arthrosc 2007;15:1130-6.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7]
[Table 1], [Table 2]
|
