|


 |
| CASE REPORT |
|
| Year : 2012 | Volume
: 4
| Issue : 1 | Page : 50-52 |
|
|
Genitourinary plexiform neurofibroma mimicking sacrococcygeal teratoma
Abdulrasheed A Nasir1, Lukman O Abdur-Rahman1, Kazeem O. O. Ibrahim2, Muideen A Adegoke1, Joselp K Afolabi3, James O Adeniran1
1 Department of Surgery, Paediatrics Surgery Division, University of Ilorin Teaching Hospital, PMB 1459, Ilorin, Nigeria
2 Department of Pathology, Paediatrics Surgery Division, University of Ilorin Teaching Hospital, PMB 1459, Ilorin, Nigeria
3 Department of Paediatrics, University of Ilorin Teaching Hospital, PMB 1459, Ilorin, Nigeria
| Date of Web Publication | 5-Sep-2012 |
Correspondence Address:
Abdulrasheed A Nasir
Paediatric Surgery Unit, Department of Surgery, University of Ilorin Teaching Hospital, PMB 1459, Ilorin
Nigeria
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.100356

 Abstract Abstract | | |
Neurofibromatosis is a common inherited autosomal dominant disease, but genitourinary neurofibroma is rare. The unpredictable nature of neurofibromas has a serious impact on the quality of life of patients, and their management is challenging for clinicians. We present a 9-year-old girl with plexiform neurofibroma of genitourinary system associated with pulmonary hypertension, masquerading as sacrococcygeal teratoma. Intraoperative finding and histological examination of the resected tumor confirmed the diagnosis. Keywords: Genitourinary, plexiform neurofibroma, pulmonary hypertension, sacrococcygeal tumor
How to cite this article:
Nasir AA, Abdur-Rahman LO, Ibrahim KO, Adegoke MA, Afolabi JK, Adeniran JO. Genitourinary plexiform neurofibroma mimicking sacrococcygeal teratoma. J Surg Tech Case Report 2012;4:50-2 |
How to cite this URL:
Nasir AA, Abdur-Rahman LO, Ibrahim KO, Adegoke MA, Afolabi JK, Adeniran JO. Genitourinary plexiform neurofibroma mimicking sacrococcygeal teratoma. J Surg Tech Case Report [serial online] 2012 [cited 2016 Jun 10];4:50-2. Available from: http://www.jstcr.org/text.asp?2012/4/1/50/100356 |
 Introduction Introduction | |  |
Neurofibromatosis type 1 (NF1) is a common inherited autosomal dominant disease with incomplete penetrance, reported in approximately 1 in 3000 individuals. [1] Although some features of NF1, such as café-au-lait spots and Lisch nodules, are clinically silent, neurofibromas cause a significant degree of morbidity, mortality, and cosmetic disfigurement. Childhood through early adulthood is a vulnerable period for the growth of these lesions. These tumors take on different morphologies, grow at variable rates, and occur in multiple locations. Symptoms arise as neurofibromas enlarge, compressing and distorting local structures. The unpredictable nature of neurofibromas has a serious impact on the quality of life of patients with NF1, and their management is challenging for clinicians. [2] Of all the manifestations of neurofibromatosis, plexiform neurofibroma is one of the most difficult to treat. With a tendency to diffusely affect entire networks of nerves, the extent of involvement is at times difficult, if not impossible, to assess. [3] Genitourinary neurofibroma is rare with fewer than 40 pediatric cases of genitourinary neurofibromatosis reported in the literature, most of them associated with generalized neurofibromatosis, with boys being affected nearly twice as often as girls. [3],[4]
We present a case of plexiform neurofibromatosis involving the uterus, bladder, perianal region, and external genitalia, associated with pulmonary hypertension in a young girl, initially diagnosed as sacrococcygeal teratoma.
 Case Report Case Report | |  |
A 9-year-old girl referred on account of a suspected sacrococcygeal teratoma presented at our center with a progressively increasing sacrococcygeal mass since birth and lower abdominal swelling of 2 years duration. She also had dyspnea, cough, and fatigue. Her mother had multiple café-au-lait spots and nodules on her skin.
The girl had café-au-lait pigmentations over her trunk with a slightly mobile, suprapubic mass and a sacral mass which extended to the perineum, involving the vulva [Figure 1]. Abdominal ultrasound scan showed hepatomegaly and bilateral hydrocalycosis. Echocardiography revealed dilated cardiomyopathy with severe systolic dysfunction and pulmonary hypertension. Magnetic resonance imaging (MRI) of the pelvic region showed numerous soft tissue masses involving the bladder, uterus, and rectum [Figure 2]. An initial diagnosis of malignant sacrococcygeal teratoma with high-output cardiac failure was made. She was managed out of cardiac failure and was transfused with 2 pints of blood. An incision biopsy showed a schwannoma and exploratory laparotomy revealed an infiltrating tumor involving the entire wall of the bladder [Figure 3], uterus, both Fallopian tube More Detailss, the distal rectum, and anus. She had debulking of the sacrococcygeal and the perineal tumor. Histology showed numerous nerve bundles with proliferating Schwann cells and fibroblasts. Patient developed progressive respiratory distress and died of cardiac failure on the 4 th postoperative week. Autopsy was refused.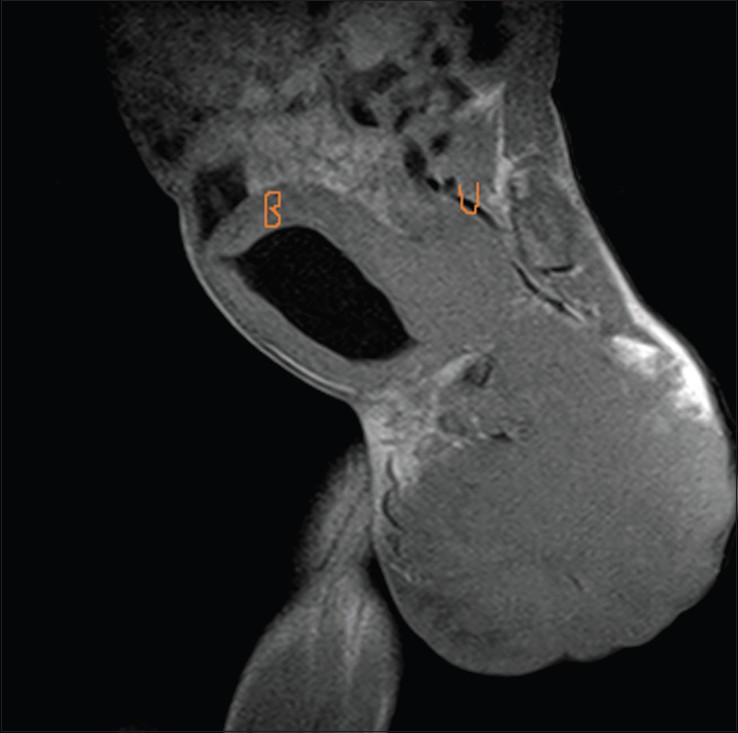 | Figure 2: Magnetic resonance imaging. The sagittal view shows a
tumor involving the bladder (B) and the uterus (U)
Click here to view |
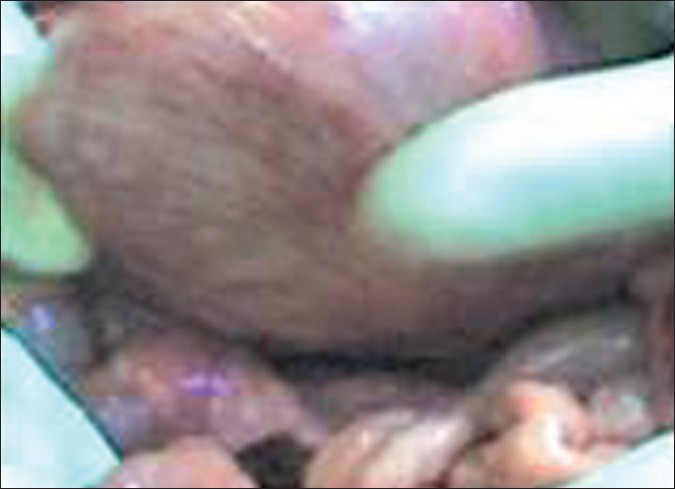 | Figure 3: Intraoperative findings showing the tumor involving the bladder
Click here to view |
 Discussion Discussion | |  |
NF1 is a common disorder of dysregulated tissue growth secondary to mutations in the tumor suppressor gene NF1. [5] Visceral (extracutaneous) involvement is seen in less than 1% of patients with neurofibromatosis. The gastrointestinal tract and the urinary bladder are the most frequently cited locations of visceral involvement. [6] However, rare reports exist describing neurofibromas, either solitary or diffuse, involving various sites in the female genital tract, the vulva, being the most common. [3],[4],[6] Diffuse plexiform neurofibroma involving the genitourinary system (GUS) is uncommon. [3] Pessin and Bodian theorized that the plexiform neurofibroma involving the bladder is derived from the vesicoprostatic plexus in males and the urethrovaginal plexus in females. [7] Variable involvement of different segments of the plexus translates into a variable constellation of signs, symptoms, and radiographic findings. Volume of disease does not strictly correlate with the degree of symptomatology. [3] This may explain why our patient was asymptomatic for 9 years. More extensive disease can present as a palpable abdominal mass causing compression that led to pain as the presenting symptom which is present in this case. Ultimately, the most damaging effect of the tumor is obstruction of the bladder neck or the lower ureter, resulting in unrecognized, progressive renal impairment. [3]
The differential diagnosis of genitourinary neurofibroma includes teratoma, meningocele, and benign vascular tumors (e.g. lymphagiomas). Typically, sacrococcygeal teratomas are seen as a visible mass at birth, making the diagnosis obvious. Lesion with a large intrapelvic component may cause urinary obstruction. Teratoma of vulva and perianal teratoma have been reported. [8],[9] Plain radiograph of pelvis may show calcification in the tumor. In cases where diagnosis is not certain, biopsy of the tumor will be helpful. Meningocele usually occurs cephalad to the sacrum and is covered with dura, but sometimes it is covered with skin. Examination of the patient with gentle pressure on the mass will reveal a bulging fontanelle, which helps to establish diagnosis. Intrapelvic component may also cause urinary obstruction.
Vascular tumors are rarely found in the female genital urinary tract. Most of the vascular tumors are incidental findings due to their small size and asymptomatic nature. However, large lesions are present clinically, with features mimicking the common gynecological tumors, even on ultrasonographic examination. [10] A lymphangioma has to be differentiated from a teratoma by looking for a prominent vascular component, hemangioma and an adenomatoid tumor. The contents in the cystic spaces, the characteristic morphology with the lymphocytic infiltrates, and immunohistochemistry may help in differentiating these conditions in the difficult cases. Extraperineal extension of lymphagioma to adjacent inguinal, abdominal, and pelvic regions is possible.
NF1-associated vasculopathies are heterogeneous and appear to contribute to the mortality of children and young adults. [7] Pulmonary arterial hypertension (PAH) in patients with NF1 is hypothesized to be secondary to this underlying vasculopathy. [5]
The spectrum of urologic presentation includes urinary frequency or urgency, and hematuria with or without a palpable abdominal or pelvic mass. Once a plexiform neurofibroma involving the lower urinary tract is suspected, it is important to define the extent and nature of the lesion with appropriate radiographic evaluation including computerized axial tomography (CAT) scan and/or MRI. [3] MRI was very useful in our patient showing multiple visceral involvement. With such a diversity of signs and symptoms in this disease, patient management must be individualized. Most patients with plexiform neurofibroma of GUS will eventually develop severe refractory symptoms and require surgery. [3] Urinary diversion may be necessary in some patients. Long-term outcome of surgical management has been disappointing, especially in children with expanding and symptomatic plexiform neurofibromatosis, who must bear the burden of plexiform growth for a lifetime. [2]
The prognosis is generally good in patients with von Recklinghausen disease, but the course is occasionally complicated by pulmonary hypertension. [5],[11] All the four patients reported by Stewart et al. died of either respiratory failure or presumed cardiac failure. [5] Pulmonary hypertension is therefore a major determinant of the morbidity and mortality in patients with von Recklinghausen disease. Our patient is of interest because the diagnosis of neurofibromatosis was not made early due to late presentation and limited experience.
Patients with multiple café-au-lait spots and sacrococcygeal mass with genitalia enlargement should be evaluated for neurofibromatosis of the genitourinary tract.
 References References | |  |
| 1. | Clark SS, Marlett MM, Prudencio RF, Dasgupta TK. Neurofibromatosis of the bladder in children: Case report and literature review. J Urol 1977;118:654-6. 
[PUBMED] |
| 2. | Rosser T, Packer RJ. Neurofibromas in children with neurofibromatosis 1. J Child Neurol 2002;17:585-91. 
[PUBMED] |
| 3. | Kaefer M, Adams MC, Rink RC, Keating MA. Principles in management of complex pediatric genitourinary plexiform neurofibroma. Urology 1997;49:936-40. 
[PUBMED] |
| 4. | Pascual-Castroviejoa I, Lopez-Pereirab P, Savastac S, Lopez-Gutierrezd JC, Lagoe CM, Cisternino M. Neurofibromatosis type 1 with external genitalia involvement presentation of 4 patients. J Pediatr Surg 2008;43:1998-2003. 
|
| 5. | Stewart DR, Cogan JD, Kramer MR, Miller WT Jr, Christiansen LE, Pauciulo MW, et al. Is pulmonary arterial hypertension in neurofibromatosis type 1 secondary to a plexogenic arteriopathy? Chest 2007;132:798-808. 
[PUBMED] |
| 6. | Gordon MD, Weilert M, Ireland K. Plexiform neurofibromatosis involving the uterine cervix, endometrium, myometrium, and ovary. Obstet Gynecol 1996;88 (4 Pt 2):699-701. 
|
| 7. | Pessin JI, Bodian M. Neurofibromatosis of the pelvic autonomic plexuses Br J Urol 1964;36:510-8. 
|
| 8. | Cakmak M, Savas C, Ozbasar D, Candir O, Kaya H, Caðlayan F. Congenital vulvar teratoma in a newborn. J Pediatr Surg 2001;36:620-1. 
|
| 9. | Jona JZ. Congenital anorectal teratoma. Report of a case. J Pediatr Surg 1996;31:709-10. 
[PUBMED] |
| 10. | Andola US, Andola SK. Vascular tumours of the female genital tract: A clinicopathologic study of 11 cases. J Clin Diagnostic Res 2012;5:1241-6. 
|
| 11. | Aoki Y, Kodama M, Mezaki T, Ogawa R, Sato M, Okabe M, et al. Von Recklinghausen disease complicated by pulmonary hypertension. Chest 2001;11:1606-8. 
|
[Figure 1], [Figure 2], [Figure 3]
|