|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2015 | Volume
: 16
| Issue : 1 | Page : 15-19 |
|
Pelvi-ureteric junction obstruction in adults in a resource limited environment: Causes, features and outcome of treatment
Augustine O Takure1, Sikiru A Adebayo1, Patience T Sotunmbi2, Linus I Okeke1, Emiola O Olapade-Olaopa1, Olayiwola B Shittu1
1 Department of Surgery, College of Medicine, University of Ibadan and University College Hospital, Ibadan, Nigeria
2 Department of Anaesthesia, College of Medicine, University of Ibadan and University College Hospital, Ibadan, Nigeria
| Date of Web Publication | 8-Oct-2015 |
Correspondence Address:
Augustine O Takure
Department of Surgery, College of Medicine, University of Ibadan and University College Hospital, Ibadan
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/1595-1103.166885

Objective: To report our experience with the management and outcome of treatment of adults with pelvi-ureteric junction(PUJ) obstruction
Subjects and Methods: This was a retrospective study of adults with PUJ obstruction from January 2009 to December 2013. The study was conducted at a Tertiary Teaching Hospital in Ibadan in Nigeria. All adults with clinical features and radiological evidence of PUJ obstruction were included. Some patients had non operative treatment while others had open surgical treatment. The main outcome of treatment was measured by the relief of symptoms. We are not aware of previous report of the management of PUJ obstruction in adults in Nigeria.
Results: Eighteen adult patients were treated. The mean age was 39 ± 11.2 standard deviation years (range 20-65 years). Seventy-two percent presented with loin pain. Thirteen of these patients were treated surgically, and 5 were treated nonoperatively. The operation findings were narrow but patent PUJ that barely admit a probe due to intrinsic muscle fibrosis in six patients, aberrant crossing vessels in 3, severely hydronephrotic kidneys in 3 and one impacted PUJ calculus. Fifty percent of patients had open dismembered pyeloplasty, simple nephrectomy (16.7%) while combined pyelolithotomy and Foley Y-V plasty (5%). All surgically treated patients were pain-free as at last time of review.
Conclusion: Intrinsic muscle fibrosis and aberrant crossing vessels are the most common causes of PUJ obstruction in adults. Open pyeloplasty is still the main stay of treatment in our environment with satisfactory symptomatic relief. Keywords: Adults, Ibadan, open pyeloplasty, pelvi-ureteric junction obstructions
How to cite this article:
Takure AO, Adebayo SA, Sotunmbi PT, Okeke LI, Olapade-Olaopa EO, Shittu OB. Pelvi-ureteric junction obstruction in adults in a resource limited environment: Causes, features and outcome of treatment. Niger J Surg Res 2015;16:15-9 |
How to cite this URL:
Takure AO, Adebayo SA, Sotunmbi PT, Okeke LI, Olapade-Olaopa EO, Shittu OB. Pelvi-ureteric junction obstruction in adults in a resource limited environment: Causes, features and outcome of treatment. Niger J Surg Res [serial online] 2015 [cited 2018 Jul 23];16:15-9. Available from: http://www.njsrjournal.org/text.asp?2015/16/1/15/166885 |
| Introduction | |  |
Pelvi-ureteric junction (PUJ) obstruction also referred to as uretero-pelvic junction (UPJ) obstruction is the functional or anatomic obstruction to urine flow from the renal pelvis into the ureter at the anatomic junction between the pelvis of the kidney and ureter. It could be due to intrinsic neural/myogenic failure with an aperistaltic segment, kinks, bands, high insertion of the ureter, and aberrant vessels whose roles are debatable.[1] PUJ obstruction may be acquired when it may be due to impacted renal pelvic stone.[2] In adults, the presentation is usually late in adolescence when the clinical features are loin pain, loin swelling, or hematuria. In patients with solitary kidney or those with bilateral obstruction, they may present with features of chronic renal impairment.[3],[4]
PUJ obstruction is commonly treated by open pyeloplasty and the various techniques, which is dependent on the extent of the renal pelvis dilatation and the location of the pelvis, whether intra-renal or extra-renal. The common techniques include dismembered pyeloplasty also referred to as Anderson-Hynes pyeloplasty, Foley Y-V plasty and Culp–Deweerd pyeloplasty. These techniques are usually done via extraperitoneal flank approach, often leading to a long hospital stay.[2]
With the advent of the first laparoscopic pyeloplasty by Schuessler et al. in 1993, increasing the number of patients with PUJ obstruction are now satisfactorily treated by this approach. The outcome of treatment by open pyeloplasty and laparoscopic pyeloplasty are comparable 91% versus 90%.[5],[6] The introduction of robotic-assisted pyeloplasty has further improved the outcome of treatment.[7],[8],[9] The outcome of any surgical treatment is either subjective based on patients assessment of their symptoms or objective where postoperative radionuclide tests such as diethylenetriaminepentaacetic (DTPA) that assess glomerular function, mercaptoacetyltriglycine that assess renal tubular function or dimercaptosuccinic acid that assess renal parenchymal damage and scarring.
Minimal access techniques have also been described for the treatment of PUJ obstruction this includes antegrade or retrograde endopyelotomy using laser and hot wire retrograde balloon dilatation can also be done. Percutaneous antegrade endopyelotomy (PAE) have comparable success rate to open pyeloplasty. It, however, advocated that PAE should be used as salvage procedure following failed open or laparoscopic surgery.[10],[11] We are not aware of previous report of PUJ obstruction in adults in Nigeria, hence, we present our experience of the causes, clinical and radiological features, and the outcome of the treatments offered to adults with this surgical disease in a tertiary teaching hospital.
| Subjects and Methods | |  |
Study setting
The study was in a Tertiary Teaching Hospital in Ibadan, Nigeria.
Study definition
All adults with symptomatic PUJ obstruction were included in the study. The selection criteria for nonoperation and operation were all patients with clinical features of loin pain and swelling had initial nonoperative treatment with intravenous fluids, alpha-receptor blocker, and analgesic such as nonsteroidal anti-inflammatory drugs diclofenac sodium. Some of this patient did not turn up for scheduled surgery. They possible had gone elsewhere for treatment, or they could not afford further surgical treatment. While those with clinical features, abdominal ultrasonography, intravenous urography (IVU), computed tomographic (CT), and DTPA renogram features of PUJ obstruction and showed up at follow-up had surgical treatment namely open pyeloplasty, with or without pyelolithotomy or nephrectomy.
Study population
A total of 18 adults with PUJ obstruction seen in the study period were included in the study.
Study design
This was a retrospective study of adults with PUJ obstruction between January 2009 and December 2013.
Data collection
The data were retrieved from the audit book of Urology Division and the case files of the 18 adults treated in the period of study. The focus was on the clinical features, which were the side of complaint, loin pain and loin swelling. The investigations are done were abdominal ultrasound, IVU, serum electrolyte, urea and creatinine, urine microscopy, culture and sensitivity, CT, and DTPA. Others were the type of treatment (nonoperative or operative), the operation findings and the outcome of treatment with an emphasis on relief of symptoms.
Limitations of the study
The limitation was that diuretic renogram which is preferred to assess the persistence of obstruction in adults with persistent loin pain after surgery was not initially available in our environment.
Data analysis
Data were analyzed using the simple statistic of mean and percentages.
| Results | |  |
A total of 18 adults who had PUJ obstruction were managed. The mean age was 39 years with a standard deviation of 11.2 years. Fifty-eight percent were males while 56% of PUJ obstructions were found on the left side. Seventy percent presented with loin pain, and 28% had loin swelling.
All the patients had abdominal ultrasound [Figure 1] that showed hydronephrosis and IVU [Figure 2] that confirmed the extent of the hydronephrosis, no flow of contrast into the proximal ureter as well as the presence of normal excretion of contrast in the contralateral kidney. | Figure 1: Abdominal ultrasound of a patient with pelvi-ureteric junction obstruction showing dilated right pelvicalyceal systems
Click here to view |
 | Figure 2: IVU of a patient with PUJ Obstruction showing dilated clubbed right pelvi-calyceal systems
Click here to view |
All the patients had abdominal ultrasound and IVU. They all had normal serum electrolyte, urea, and creatinine that were within normal limits. The CT in a single patient revealed the degree of hydronephrosis. DTPA in one patient show split renal functions of 35% and 65% of the left and right kidneys with and delayed excretion from left kidney. The urine cultured in a patient yielded Eschericia coli sensitive to ciprofloxacin while the rest yielded no growth of bacteria.
In [Table 1], 5 (27.7%) of the patient were managed nonoperatively because they declined surgical option of treatment, and thus the etiology of the UPJ obstruction could not be ascertained. However, of the 13 who had surgery, 9 were open dismembered pyeloplasty with operation and histologic findings of narrowed ureter that was patent to probe, had intrinsic muscle fibrosis 6 (33.3%), and three patients (16.7%) had crossing aberrant vessels. Three adults had severe hydronephrosis with thinned out renal parenchyma for which simple nephrectomy was performed while combined pyelolithotomy and Foley Y-V plasty was done in 1 (5.6%) with impacted renal pelvic stone.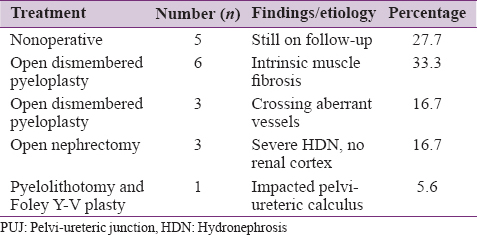 | Table 1: Treatment, operation performed and operation findings in adults with PUJ obstruction
Click here to view |
| Discussion | |  |
PUJ obstruction is a common upper urinary tract abnormality in children with 34% of them seen present in utero.[12] The condition is also not uncommon in adults.
The mean age of the condition in our present study is in the third decade which is consistent with other studies in Jos, Nigeria,[13] Saudi Arabia,[5] New York and Indiana in the USA.[7] However, this is in contrast with the findings in patients in Washington DC, where the mean age of those affected is in the fourth decade.[9]
Contrary to some studies that reported a higher incidence of PUJ obstruction in females,[7],[9],[12],[13],[14] in this study, there was slight male preponderance, that is, similar to study from Saudi Arabia. The possible explanation for the gender difference is not known.[2]
The left side (56%) is slightly more affected in our series a finding, that is, similar to worldwide observation.[2],[12] The reason why the patient would present with right or left PUJ obstruction is not clear.
As in other reports of adult PUJ obstruction, the majority (72%) of these patients presented with loin pain.[13] There was no adult with a renal impairment in our study neither was any patient with incidental imaging feature of significant asymptomatic hydronephrosis while on evaluation for other abdominal conditions.[3],[4] Patient often tend to present at the hospital whenever there is no immediate explanation for the observed pain though Hellenthal et al.,[3] reported an adult with silent PUJ obstruction complicated by renal impairment.
In this study as with other report, abdominal ultrasonography without pulsed Doppler technology and IVU were both useful in assessing the degree of hydronephrosis.[15]
Contrast three-dimensional CT scan as compared to two-dimensional CT is very useful in establishing the anatomic abnormality at PUJ obstruction and could detect aberrant crossing vessels. This imaging study could completely replace angiography and conventional IVU.[16] The diagnostic accuracy of CT urogram is as high as 85.2% compared to 49.2% with IVU. IVU does not identify vascular abnormality cause of hydronephrosis.[17] This may explains why in the patients in the study who were managed nonoperatively, the etiology of the PUJ obstruction could not be ascertained. Although Wolf et al.[15] and Tayib [2] emphasized that in adult with PUJ obstruction, IVU and diuretic scintigraphy were adequate in evaluating this category of patients. It is also worthy of note that Tayib study showed that postpyeloplasty split renal function improved by 3–7% in 64% of patients while IVU only showed the disappearance of the PUJ obstruction in 20%.[2] However, Hellenthal et al.[3] reported a case that revealed the imperfection of diuretic renogram in differentiating split renal function in an adult with silent PUJ obstruction manifesting with rapid onset renal deterioration.
In this study, abdominal ultrasound and IVU were valuable in arriving at a reasonable diagnosis of PUJ obstruction in the adult population considering the limitation of resources. The other limitation in this study is in follow-up, as the degree of persistent obstruction could not be objectively assessed since this facility was not available.[2],[6],[13]
The most common cause of PUJ obstruction in this study was narrowed ureter at the PUJ that barely admitted a probe size of 5F and 6F similar to findings in children with PUJ obstruction unlike in other studies where crossing aberrant vessel is often the cause in the adults. This vascular anomaly was seen in only 3 of 13 operated patients in this study. These findings further reaffirm that PUJ obstruction could be congenital but may not become symptomatic until adulthood.[18],[19]
Open pyeloplasty is the standard method of treatment for PUJ obstruction and is the most commonly used method of treatment in the United States.[20] In this study, 50% of the patients had open pyeloplasty with an overall success rate similar to that in international studies.[2],[6],[13],[21] Dismembered (Anderson Hynes) pyeloplasty was done for these patients. This technique of treatment avoids injury to the aberrant crossing renal vessels, a complication that can occur during endopyelotomy. Unilateral nephrectomy is the treatment in patients with severe hydronephrotic kidney with absent renal parenchyma.[19]
In high volume centers with PUJ obstruction, laparoscopic pyeloplasty in an adult is evolving to become the gold standard for treatment. The advantages include low morbidity, early convalescence, and comparable outcome to open pyeloplasty.[22] Uberoi et al.[23] further suggested that robotic pyeloplasty be considered by a urologist because this procedure is more precise and has a shorter learning curve. While these techniques are laudable, open pyeloplasty should still remain the standard treatment in low-resource environment. Laparoscopic and robot-assisted pyeloplasty should be encouraged particularly since several studies have shown that the subjective and objective outcome of minimal access surgery such as laparoscopic and robotic pyeloplasty is comparable to open pyeloplasty.[2],[5],[6],[7],[8],[9],[23] However, the success rate of endopyelotomy of 15–20% is less encouraging.[19]
The outcome of pain-free symptoms of 100% of postoperative patients in this study is comparable to findings in other series.[2],[6],[13]
| Conclusion | |  |
The common causes of PUJ obstruction in adults in our study were intrinsic muscle fibrosis and aberrant crossing vessels. Abdominal CT scan and DTPA were less utilized in the diagnosis of PUJ obstruction because they were not available in the earlier part of this study. Open pyeloplasty is still the mainstay of treatment in our resource-limited environment and provides a satisfactory outcome.
| References | |  |
| 1. | Kausik S, Segura JW. Surgical management of ureteropelvic junction obstruction in adults. Int Braz J Urol 2003;29:3-10.  |
| 2. | Tayib AM. Long term results of pyeloplasty in adults. Saudi Med J 2004;25:363-6.  |
| 3. | Hellenthal NJ, Thomas SA, Low RK. Rapid onset renal deterioration in an adult with silent ureteropelvic junction obstruction. Indian J Urol 2009;25:132-3.  [ PUBMED]  |
| 4. | Sepulveda L, Rodrigue F. Giant hydronephrosis - A late diagnosis of ureteropelvic junction obstruction. World J Nephrol Urol 2013;2:33-5.  |
| 5. | Schuessler WW, Grune MT, Tecuanhuey LV, Preminger GM. Laparoscopic dismembered pyeloplasty. J Urol 1993;150:1795-9.  |
| 6. | Bauer JJ, Bishoff JT, Moore RG, Chen RN, Iverson AJ, Kavoussi LR. Laparoscopic versus open pyeloplasty: Assessment of objective and subjective outcome. J Urol 1999;162:692-5.  |
| 7. | Palese MA, Munver R, Phillips CK, Dinlenc C, Stifelman M, DelPizzo JJ. Robot - Assisted laparoscopic dismembered pyeloplasty. JSLS 2005;9:252-7.  |
| 8. | Conley SP, Lee BR. Adult Laparoscopic and Robotic-Assisted pyeloplasty for ureteropelvic junction obstruction. In: Robotic and Laparoscopic Reconstructive Surgery in Children and Adults, Current Clinical Urology. M.C. Ost (ed.), LLCL: Springer Science and Media; 2011. p. 85-92.  |
| 9. | Thom MR, Haseebuddin M, Roytman TM, Benway BM, Bhayani SB, Figenshau RS. Robot-Assisted pyeloplasty: Outcomes for primary and secondary repairs, a single institution experience. Int Braz J Urol 2012;38:77-83.  |
| 10. | Elabd SA, Elbahnasy AM, Farahat YA, Soliman MG, Taha MR, Elgarabawy MA, et al. Minimally-invasive correction of ureteropelvic junction obstruction: Do retrograde endo-incision techniques still have a role in the era of laparoscopic pyeloplasty? Ther Adv Urol 2009;1:227-34.  |
| 11. | Rukin NJ, Ashdown DA, Patel P, Liu S. The role of percutaneous endopyelotomy for ureteropelvic junction obstruction. Ann R Coll Surg Engl 2007;89:153-6.  |
| 12. | Tam JC, Hodson EM, Choong KK, Cass DT, Cohen RC, Gruenewald SM, et al. Postnatal diagnosis and outcome of urinary tract abnormalities detected by antenatal ultrasound. Med J Aust 1994;160:633-7.  |
| 13. | Ramyil VM, Dakum NK, Ogwuche EI. The management of upper urinary tract obstruction in resource poor settings. Afr J Urol 2008;13:30-6.  |
| 14. | Siqueira TM Jr, Nadu A, Kuo RL, Paterson RF, Lingeman JE, Shalhav AL. Laparoscopic treatment for ureteropelvic junction obstruction. Urology 2002;60:973-8.  |
| 15. | Wolf JS Jr, Siegel CL, Brink JA, Clayman RV. Imaging for ureteropelvic junction obstruction in adults. J Endourol 1996;10:93-104.  |
| 16. | Lawler LP, Jarret TW, Corl FM, Fishman EK. Adult ureteropelvic junction obstruction: Insights with three-dimensional multi-detector row CT. Radiographics 2005;25:121-34.  |
| 17. | Xie C, Guo J, Wang G, Wang H. Comparison between intravenous urography and computed tomography in diagnosing ureteropelvic junction obstruction. Nephrourol Mon 2011;3:258-63.  |
| 18. | Grasso M, Caruso RP, Phillips CK. UPJ obstruction in the adult population: Are crossing vessels significant? Rev Urol 2001;3:42-51.  |
| 19. | Carr MC, El-Ghoneimi A. Anomalies and surgery of the ureteropelvic junction in children. In: Wein AJ, Kavoussi LR, Norvick AC, Partin AW, Peters CA, editors. Campbell-Walsh Urology. 9 th ed. Philadelphia: WB Saunders Elsevier; 2007. p. 3359-82.  |
| 20. | Fallon E, Ercole B, Lee C, Best S, Skenazy J, Monga M. Contemporary management of ureteropelvic junction obstruction: Practice patterns in Minnesota. J Endourol 2005;19:41-4.  |
| 21. | Eden CG. Minimally invasive treatment of ureteropelvic junction obstruction: A critical analysis of results. Eur Urol 2007;52:983-9.  |
| 22. | Luke P. The gold standard for the treatment of uncomplicated adult ureteropelvic junction obstruction. Can Urol Assoc J 2008;2:393.  |
| 23. | Uberoi J, Disick GI, Munver R. Minimally invasive surgical management of pelvic-ureteric junction obstruction: Update on the current status of robotic-assisted pyeloplasty. BJU Int 2009;104:1722-9.  |
[Figure 1], [Figure 2]
[Table 1]
|