 |
July-September 2011
Volume 5 | Issue 3
Page Nos. 61-84
Online since Monday, October 17, 2011
Accessed 16,659 times.
PDF access policy
Full text access is free in HTML pages; however the journal allows PDF access only to users from SOUTH AFRICA and paid subscribers.
EPub access policy
Full text in EPub is free except for the current issue. Access to the latest issue is reserved only for the paid subscribers.
|
| |
|
|
Show all abstracts Show selected abstracts Add to my list |
|
| ORIGINAL ARTICLES |
|
|
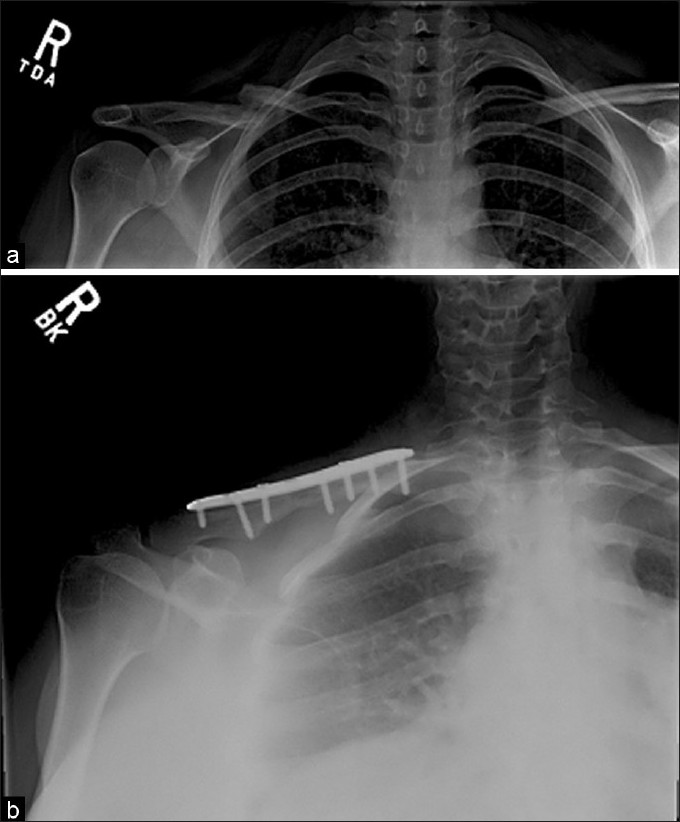  |
Open reduction and internal fixation of clavicular nonunions with allograft bone substitute |
p. 61 |
Michael D Riggenbach, Grant L Jones, Julie Y Bishop
DOI:10.4103/0973-6042.86232 PMID:22058638Background: Biologic augmentation with allograft has shown equivalent healing rates to autograft in several nonunion models. No literature exists clearly demonstrating this in the clavicle. The purpose of this study was to evaluate the healing and complication rates of clavicle nonunions treated solely with open reduction and internal fixation (ORIF) and allograft.
Materials and Methods: Nineteen clavicle nonunions treated with ORIF and allograft were evaluated retrospectively to assess healing rates and complications based on clinical symptoms and radiographic findings.
Results: For the 19 patients included and treated with ORIF and allograft, clinical follow-up averaged 15 months. Seven patients were smokers. Although complete radiographic healing was achieved in only 68% of patients, clinical success occurred in 16 (84%) patients who demonstrated full range of motion and strength without pain. The three patients who did not demonstrate full radiographic healing were completely pain free. Five patients experienced complications (26%). Two underwent hardware removal due to persistent irritation after union. Three had a persistent painful nonunion. Each of these three patients was a smoker (P=0.08). Two proceeded to union after revision fixation. The other had hardware failure, which was removed, with a persistent nonunion and did not wish any further treatment.
Conclusion: ORIF with allograft bone substitute is an acceptable treatment alternative to iliac crest bone graft for clavicle nonunions. However, we did not demonstrate equivalent healing rates to published results utilizing autograft. Smokers were identified to have a trend toward higher failure rates with ORIF augmented with allograft and therefore these patients may be better served by augmenting fixation with autograft.
Level of Evidence: IV; retrospective comparative study. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
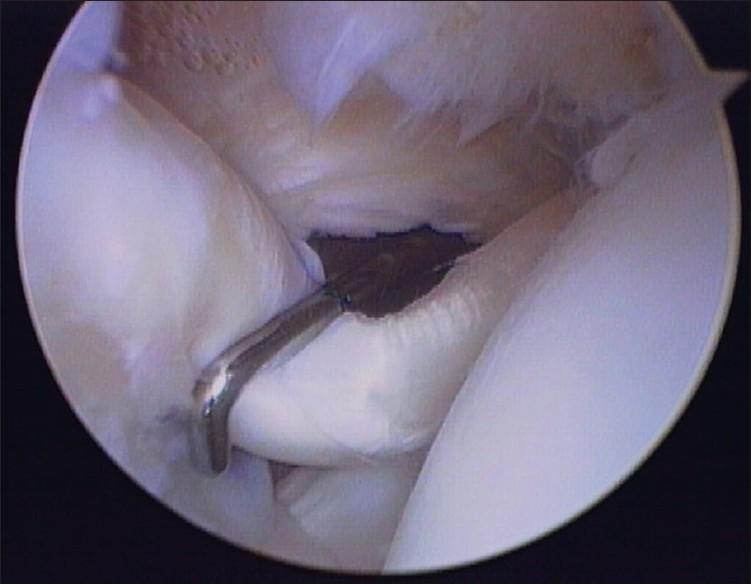  |
Arthroscopic evaluation and treatment of biceps brachii long head tendon injuries: A survey of the MOON shoulder group |
p. 68 |
Timothy Miller, Grant Jones, Moon Shoulder Group
DOI:10.4103/0973-6042.86236 PMID:22058639Context: Injuries to the biceps brachii long head tendon commonly occur in conjunction with tears in the rotator cuff and glenoid labrum. Consensus on treatment of varying levels of severity is undetermined.
Settings and Design: We surveyed members of the Multicenter Orthopedic Outcomes Network (MOON) Shoulder Group, to determine a consensus on arthroscopic grading and treatment.
Aims: We hypothesized that the Lafosse classification system would show a high level of inter- and intraobserver agreement regarding grading/treatment.
Materials and Methods: Arthroscopic videos of 30 patients determined to have biceps brachii long head tendon injuries were viewed by 13 surgeons. The surgeons graded the severity of the injury macrostructure based on the Lafosse classification system and chose from a list of treatment options. Four months later the same surgeons viewed the same videos and repeated the survey.
Statistical Analysis Used: Analysis with weighted and non-weighted Kappa values was performed to determine intra- and interobserver reliability for severity grading and to determine the preferred treatments for each level of severity.
Results: Intraobserver reliability testing for the Lafosse system showed substantial agreement after two rounds (81.28%, K=0.7006). Interobserver testing demonstrated substantial agreement for Grade 0 (K=0.7152), fair agreement for Grade 1 (K=0.3803), and moderate agreement for Grade 2 (K=0.5156). Combined responses recommended no surgical treatment for 95.4% of the lesions classified as grade 0 (62/65). No surgical treatment was recommended for Grade 1 lesions in 24.1% of the cases (35/145), debridement in 38.6% (56/145), and tenotomy or tenodesis in 37.2% (54/145). Evaluators preferred tenotomy or tenodesis for 98.3% of the Grade 2 lesions (177/180).
Conclusions: Analysis of the Lafosse system indicated substantial intraobserver reliability for all grades. As Grades 1 and 2 showed only fair and moderate agreement, a need for a reliable grading system still exists. Grade 2 lesions should be treated with tenotomy or tenodesis. A preferred treatment for Grade 1 lesions could not be determined given the high variability of responses. Higher-powered surveys may help determine the ideal treatment of Grade 1 injuries. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (4) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| CASE REPORTS |
 |
|
|
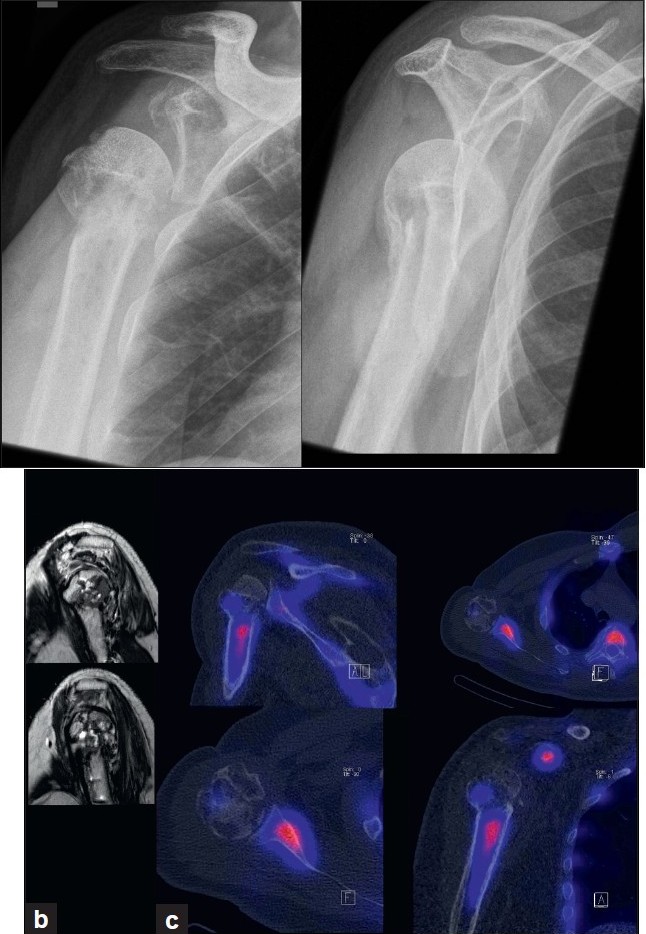  |
Combined single photon emission computerized tomography and conventional computerized tomography: Clinical value for the shoulder surgeons? |
p. 72 |
Michael T Hirschmann, Rahel Schmid, Ranju Dhawan, Jiri Skarvan, Helmut Rasch, Niklaus F Friederich, Roger Emery
DOI:10.4103/0973-6042.86242 PMID:22058640With the cases described, we strive to introduce single photon emission computerized tomography in combination with conventional computer tomography (SPECT/CT) to shoulder surgeons, illustrate the possible clinical value it may offer as new diagnostic radiologic modality, and discuss its limitations. SPECT/CT may facilitate the establishment of diagnosis, process of decision making, and further treatment for complex shoulder pathologies. Some of these advantages were highlighted in cases that are frequently seen in most shoulder clinics. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (12) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
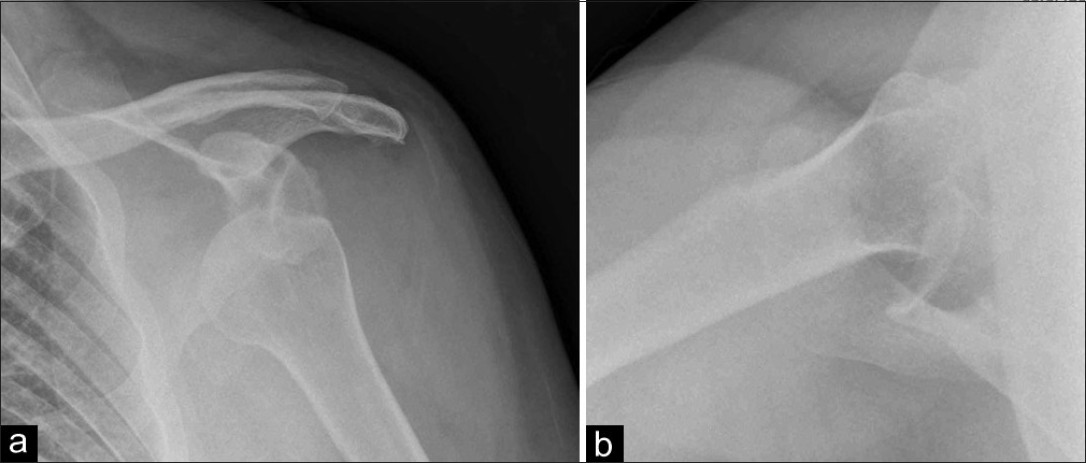  |
Innovative use of computer-assisted tomography in the management of an irreducible anterior shoulder dislocation |
p. 77 |
Rajpal S Nandra, Harpal Uppal, Gulraj Matharu, Stuart Brooks, Kapakuntra Srinivasan
DOI:10.4103/0973-6042.86245 PMID:22058641Anterior dislocation of the shoulder is a common injury which is often reduced in the emergency department, without specialist orthopedic input. We report a case of an irreducible locked anterior glenohumeral dislocation with impaction of the humeral head onto the antero-inferior glenoid rim and subsequent generation of a Hill-Sachs lesion. To our knowledge, we describe the first reported case of using computer-assisted tomography to generate a sequence of movements to safely disimpact the locked dislocation without causing further iatrogenic injury or a fracture through the humeral articular surface. This novel image-assisted closed reduction technique spared the patient from the morbidity associated with performing open reduction surgery. At 6-month follow-up, the patient reported no re-dislocations, returned to work and had excellent range of motion. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
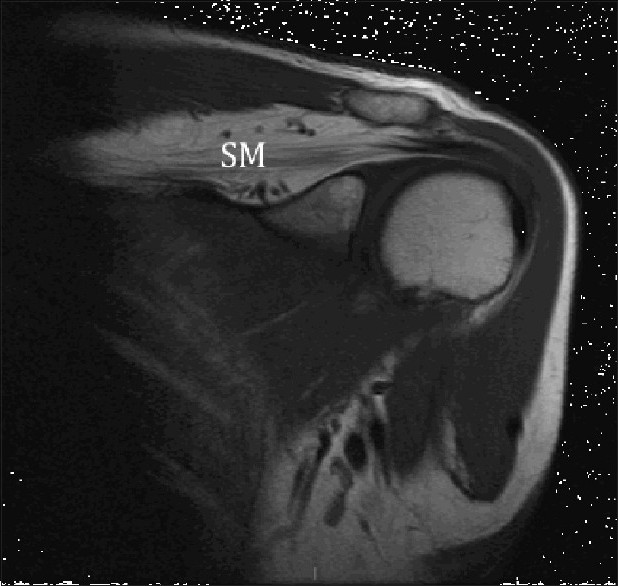  |
Isolated supraspinatus muscle atrophy and fatty infiltration associated with recurrent anterior shoulder instability: A case report and review of the literature |
p. 81 |
Abdulaziz Z Alomar, Tom Powell, Mark L Burman
DOI:10.4103/0973-6042.86246 PMID:22058642Supraspinatus muscle atrophy and fatty infiltration are two distinct muscle abnormalities which can be seen after a chronic massive tear or suprascapular neuropathy. Isolated supraspinatus muscle denervation due to suprascapular nerve injury after shoulder dislocation is extremely rare.
We report on a patient who developed isolated supraspinatus muscle atrophy and fatty infiltration after traumatic anterior shoulder instability. Possible explanations and etiologies of this rare condition are discussed in this report. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
