|
Show all abstracts Show selected abstracts Add to my list |
|
| EDITORIAL |
|
|
|
Bioengineering Tissue for Organ Repair, Regeneration, and Renewal |
p. 77 |
Ismaila A Mungadi
DOI:10.4103/2006-8808.110247 PMID:23741579 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| REVIEW ARTICLE |
 |
|
|
|
Diagnosis and Management of Adnexal Masses in Pregnancy |
p. 79 |
Ibrahim Adamu Yakasai, Lawal Abdullahi Bappa
DOI:10.4103/2006-8808.110249 PMID:23741580Widespread use of ultrasound in early pregnancy has led to the detection of incidental adnexal masses more frequently. This article reviews the diagnosis and management options for adnexal masses in pregnancy. The availability of high-resolution ultrasound has made observation to be a viable option in some cases. However, for those masses suspicious of malignancy, at risk of torsion, rupture, or clinically symptomatic, surgical treatment is warranted. Laparoscopy has been successfully used in pregnancy and is safe in experienced and trained hands in properly equipped units. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (3) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| ORIGINAL ARTICLE |
 |
|
|
|
Patient Satisfaction Following Minimally Invasive Repair of Pectus Excavatum: Single Surgeon Experience |
p. 86 |
Anupama Barua, Vinay P Rao, Biplab Barua, Andrzej Majewski
DOI:10.4103/2006-8808.110253 PMID:23741581Background: Pectus excavatum (PE) is the most common chest wall deformity in adolescent life. Nuss procedure is a well-established technique for the repair of PE. The indication for correction is mainly medical aesthetic. Advantages of Nuss over conventional methods include reduced length of hospital stay, smaller incisions, and absence of need for osteochondrectomies. Here, we describe our experience with this procedure. Materials and Methods: This was a retrospective study of patients who underwent Nuss procedure by a single surgeon between 2006 and 2010 in a regional center. Indications for surgery included the following: Progressive deformity and psychological stress. All patients underwent chest X-ray and pulmonary function testing. A standard Nuss procedure was performed using a single bar. Patients' satisfaction was assessed by a questionnaire and follow-up clinic letters. Satisfaction with body image was scored on a scale of 1-10. Results: Eleven patients with PE underwent correction by Nuss procedure. Mean age of the patient was 19 years (range: 15-30). The average hospital stay was 7 days (range: 4-23 days). There was no mortality and no episodes of wound infection. In the immediate post-operative period, three patients (12.5%) were noted to have poor pain control. The post-operative course was uneventful in all cases except one patient who developed lung collapse, pleural effusion, and bar dislocation. Hundred percent of patients were satisfied with the scar. Seven patients scored 7 out of 10 on satisfaction with body image and two patients scored 6 or less. None of the patients complained of chronic pain. Conclusion: Nuss procedure is an effective method for the correction of PE. Most patients were satisfied with the outcome and none experienced chronic pain. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (3) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| SURGICAL TECHNIQUES |
 |
|
|
|
Mesh-free Ventral Rectopexy for Women with Complete Rectal and Uterovaginal Prolapse |
p. 89 |
Adedayo O Tade, Adetola O Olatunji
DOI:10.4103/2006-8808.110256 PMID:23741582Background: Mesh rectopexy may be associated with infective complications, erosion into the vagina or rectum, and disintegration or dislodgement. A mesh-free rectopexy will avoid these complications. Objective of the study was to perform mesh-free ventral rectopexy and assess its safety and effectiveness. Materials and Methods: Nine women with complete rectal and uterovaginal prolapse were treated with total abdominal hysterectomy, closure of the vaginal vault, extirpation of the pouch of Douglas and suture of anterior rectal wall to the posterior vaginal wall (ventral suture rectopexy). The ventral suture rectopexy was achieved by three pairs of interrupted silk sutures, 2.5 cm above each other, and the first pair very close to the pelvic floor. This composite structure (anterior rectal wall and posterior vaginal wall), sits astride the perineal body. Intussusception and subsequent prolapse of the sutured rectum and vaginal wall is prevented. Vaginal vault prolapse was prevented by the suture of each round ligament of the uterus to the corresponding lateral vaginal fornix. No mesh was used. Results: Nine multiparous women aged between 52 and 70 years had the procedure. The mean operative time was 135 minutes (range 110-220). The follow-up period was between 29 months and 7 years. Full continence was restored in all patients within eight weeks of the operation. Bowel habit returned to once daily in four patients and once every other day in the remaining five patients, within thirteen weeks of surgery. One patient had intermittent mucus discharge per rectum for six months. This stopped without a specific treatment. There has been no known recurrence in these nine patients. One patient developed wound infection as a complication. There was no mortality. All the patients are now asymptomatic. Conclusion: Ventral suture rectopexy is a safe and effective treatment for complete rectal prolapse in a selected group of patients. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
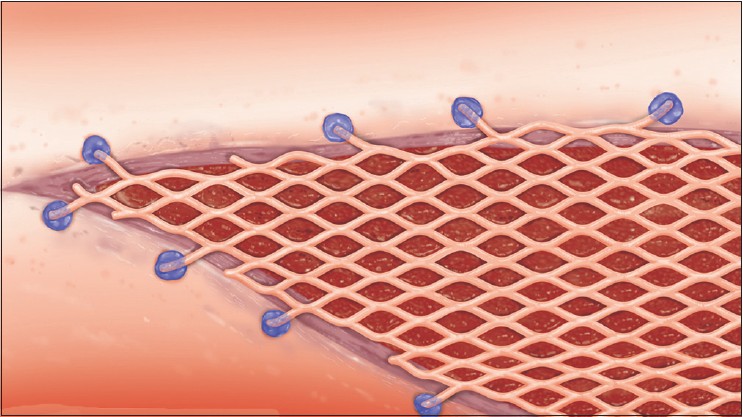  |
"The Dendritic Bonding Technique": A Newly-devised Technique for the Fixation of Mesh Skin Graft |
p. 92 |
Yoshiaki Sakamoto, Kazuo Kishi
DOI:10.4103/2006-8808.110258 PMID:23741583We describe a newly designed technique for the quick, easy, and cost-effective fixation of mesh skin grafts in a range of skin conditions and patients. We fixed the skin graft using octyl-2-cyanoacrylate (Dermabond; Ethicon), which was termed "Dendritic bonding." This technique exhibits several advantages over surgical stapling and suturing with absorbable sutures. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
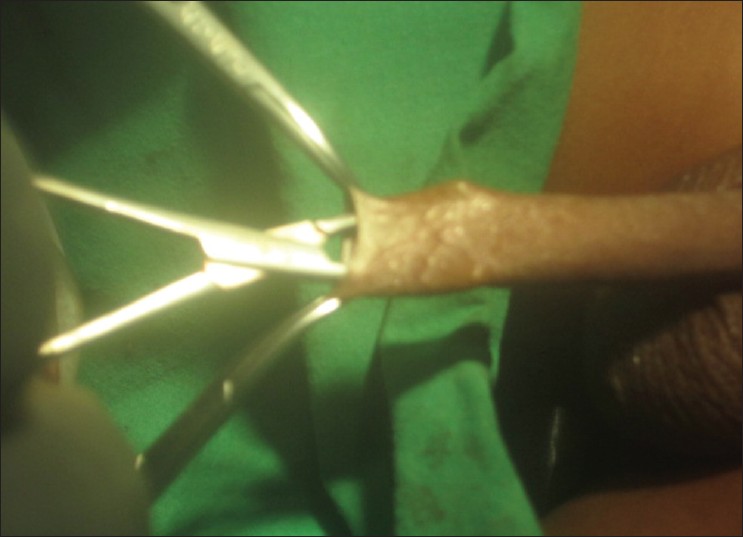  |
Dorsal Slit-Sleeve Technique for Male Circumcision  |
p. 94 |
Christopher Suiye Lukong
DOI:10.4103/2006-8808.110261 PMID:23741584Male circumcision is a commonly performed surgical procedure. There are several techniques of circumcision. The device methods are thought to have lower complication rates when compared to the open methods. The devices for circumcision may not be readily available or may be expensive. The open methods are therefore still commonly used in this setting. The dorsal slit-sleeve technique combines strategies from two open methods. The technique is described, together with its merit and demerits. This technique is feasible, safe, and the general outcome is good. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| CASE REPORTS |
 |
|
|
  |
Early Weight-bearing Using Percutaneous External Fixator for Calcaneal Fracture |
p. 98 |
Vetrivel Chezian Sengodan, Mugundhan Moongilpatti Sengodan
DOI:10.4103/2006-8808.110263 PMID:23741585Calcaneal fracture, the most common tarsal bone fracture, occurs predominantly in manual labors and subsequently has got considerable socioeconomic implications. Treatment modality which can offer early weight bearing and early return to work is therefore needed for those patients. We have used a biplanar percutaneous external fixator for treating calcaneal fractures without operative and per operative visualization of the fractures. We have treated 17 calcaneal fractures in 16 patients, 12 intra articular and five extra articular, with our percutaneous external fixator system without preoperative X-ray control or reduction. Functional outcome was measured using the American Orthopaedic Foot and ankle society Hind foot score. All fractures united with a mean of 55 days. Partial weight bearing was possible in a mean of 1.8 days and full bearing was possible in a mean of 11.6 days. All the patients were returned to their original work within six weeks. Minor infectious complications occurred in 17.6 percent of cases. The average AOFAS score at six months follow up was 83.8. We conclude that our percutaneous external fixator technique for fracture calcaneum is an effective alternative to the currently available - surgical and conservative treatment modalities especially in lower socio economic labor population who need to return to their job as early as possible. Level of Evidence - IV Case series. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (2) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
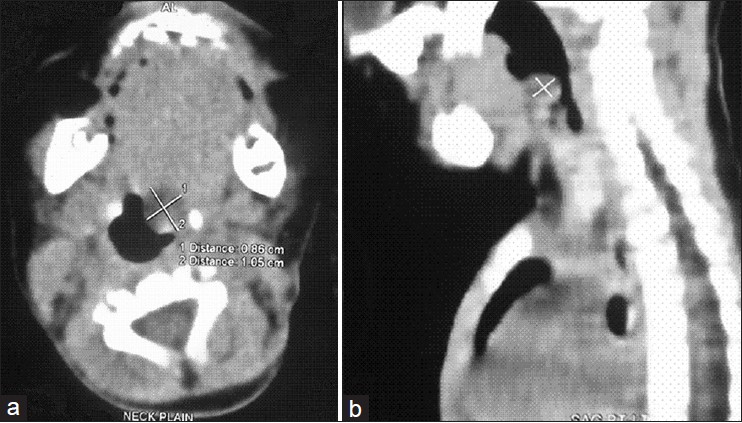
Phlebectasia of Internal Jugular Vein |
p. 103 |
Satish K Bindal, Gaurav O. P. Vasisth, Puneet Chibber
DOI:10.4103/2006-8808.110266 PMID:23741586Internal jugular phlebectasia (IJP) is a rare disease in which there is a fusiform dilatation of internal jugular vein, usually presenting as a neck mass in children. Accurate diagnosis from careful history, physical examination, and radiological study can be made. We report a 12-year-old boy with history of swelling appearing on the right side of the neck only on straining, coughing, or during a Valsalva maneuver. Diagnosis of right IJP was made. Exploration and wrapping the dilated segment in an 8-mm-diameter polytetrafluoroethylene tube graft was done. Because of its rarity, this entity is frequently ignored or misdiagnosed. This case report intends to stress the importance of keeping IJP as differential diagnosis while dealing with such a swelling to avoid invasive investigations and inappropriate treatment. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Is Aggressive Therapy the Answer for All Cases of Emphysematous Pyelonephritis: A Report of Three Cases |
p. 106 |
Sidharth Kumar, Sushanto Neogi, Kamal K Gautam
DOI:10.4103/2006-8808.110268 PMID:23741587Emphysematous Pyelonephritis (EPN) is a severe, necrotizing, life threatening infection of the renal parenchyma and management is not standardised due to scarcity of literature. We present 3 patients with this rare entity. All 3 patients were of class III on CECT findings based on Huang's classification and had more than two risk factors. Our first patient underwent percutaneous drainage of his condition upon which he recovered. The second and third patients underwent a laparotomy and nephrectomy. The second patient recovered after a stormy post operative period and the third patient died. Management of the first patient was contrary to that recommended in literature, for the other two it was as per recommendations. On successful management of our first patient without surgery and seeing no discernable benefits of surgery for our other two patients, it is possible that percutaneous drainage alone, coupled with antibiotics may be a viable strategy for managing this condition with nephrectomy being considered as a second tier option. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
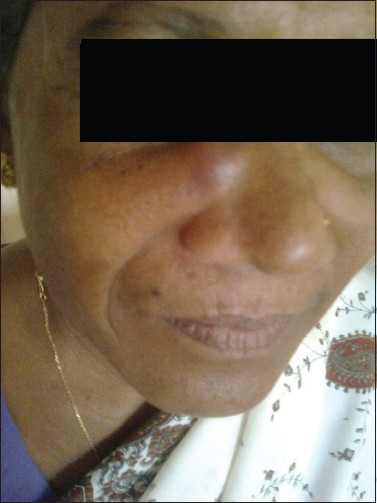  |
A Rare Case of Spindle Cell Lipoma of Nose |
p. 110 |
Deepalakshmi Tanthry, PP Devan, Kavitha Ashok Kumar, Rukma Bhandary
DOI:10.4103/2006-8808.110250 PMID:23741588We present a case report of a 45-year-old lady with history of swelling on right side of the nose since two years. On clinical examination, there was a firm swelling, 3 × 2 cm in size, just above the right nasoalar crease, nontender and mobile. Computed tomography revealed fibrous tissue over anterior surface of the right maxilla and nasal bone with mild sclerosis of the right nasal bone. Excision was done through lateral rhinotomy incision. Histopathological examination of the excised specimen revealed spindle cell lipoma which is very rare. Very few cases have been reported in the literature so far. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (2) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Follicular Thyroid Carcinoma Presenting as Massive Skull Metastasis: A Rare Case Report and Literature Review |
p. 112 |
Sanjay N Koppad, Vaibhav B Kapoor
DOI:10.4103/2006-8808.110252 PMID:23741589Follicular carcinoma of thyroid is a well differentiated thyroid malignancy. It is slow growing in nature and tends to metastasize to remote organs in advanced stage by hematogenous route. Lung and bone are the two most common sites of metastasis. In most of the reported cases of follicular thyroid carcinoma metastasizing to the skull, metastases occurred long after the diagnosis and institution of treatment for primary cancer. Very few cases have been reported with occult follicular thyroid carcinoma presenting as skull metastasis. A 48-year-old female patient presented with massive swelling in the frontal region of skull associated with swellings in occipital region. Evaluation confirmed that it is multiple metastases to skull bones from follicular thyroid carcinoma. This is a very rare presentation with such a large size of metastasis. We report this case of a metastatic follicular thyroid carcinoma presenting as massive skull tumor at our institution. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (4) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Melioidosis of Chest Wall Masquerading as a Tubercular Cold Abscess |
p. 115 |
Nelamangala Ramakrishnaiah Vishnu Prasad, Gopal Balasubramaniam, Vilvapathy Senguttuvan Karthikeyan, Ramesh Kapil Chakravarti, Krishnamachari Srinivasan
DOI:10.4103/2006-8808.110254 PMID:23741590Melioidosis caused by Burkholderia pseudomallei, an important human pathogen in the tropical regions causes protean and multisystem clinical manifestations. A 50-year-old man on treatment for pulmonary tuberculosis developed a chest wall abscess. With a suspicion of tuberculous cold abscess, pus culture was done and it revealed Burkholderia pseudomallei. He was treated with 10 days of ceftazidime and incision and drainage was done. Wound healed well and he has now completed three months of oral cotrimoxazole eradication therapy and is on follow-up without recurrence. We report this case for the unusual presentation of melioidosis and the diagnostic challenge posed due to clinical similarity with tuberculosis. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
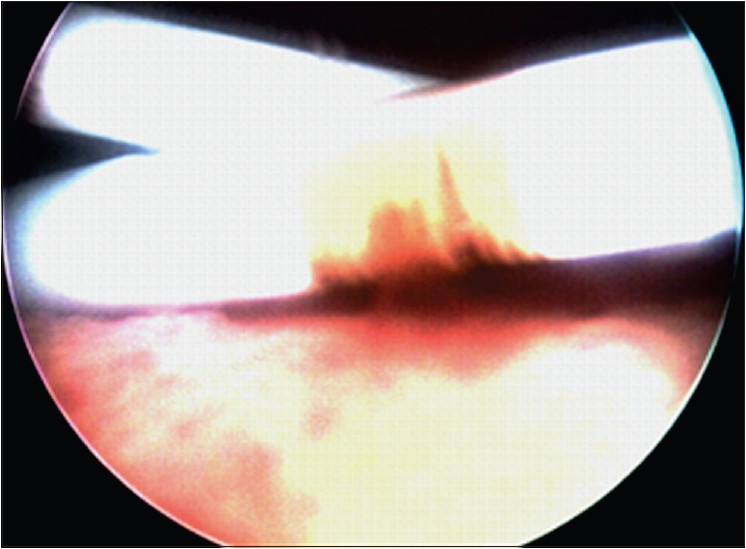
An Unusual Presentation of Vallecular Cyst with near Fatal Respiratory Distress and Management Using Conventional Laparoscopic Instruments |
p. 118 |
Sandesh V Parelkar, Jiwan L Patel, Beejal V Sanghvi, Prashant B Joshi, Subrat K Sahoo, Nandita Sampat, Sanjay N Oak, Nilam Sathe
DOI:10.4103/2006-8808.110257 PMID:23741591Vallecular cyst is a rare cause of upper airway obstruction in infants and children and presentation like acute stridor with near fatal respiratory distress is extremely rare. It is one of the rare causes of difficult intubation, during which cyst aspiration can improve the access. Vallecular cyst is commonly managed using microlaryngoscope and specialized instruments. We hereby report a method of endoscopic management of these cysts using conventional laparoscopic instruments. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Arthroscopic Bullet Removal from the Acetabulum (Hip Joint) |
p. 121 |
Jamal Al-Asiri, Ivan Wong
DOI:10.4103/2006-8808.110260 PMID:23741592Hip arthroscopy has been shown to offer minimally invasive access to the hip joint compared with standard open arthrotomy. The use of arthroscopy for diagnosing and treating disorders about the hip continues to evolve. This study describes a case that involves arthroscopic removal of a bullet from a low-velocity gunshot wound. The patient sustained a gunshot wound that entered the abdomen and traversed the small bowel, sigmoid colon then penetrated the urinary bladder before ending up in the medial wall of the acetabulum. After surgical repair of the viscus, the bullet was retrieved from the hip joint using standard arthroscopic portals and a fracture table. A number of issues led to the decision to use arthroscopy. Most importantly was the need to minimize soft tissue dissection, which was required to access the bullet, without interfering with previous wound at the suprapubic area. The risks of potential bullet fragmentation and migration, as well as a possible abdominal compartment syndrome were considered before proceeding. Arthroscopy allowed adequate inspection of the articular surface, irrigation of the joint, and removal of the foreign body while avoiding an invasive arthrotomy with its associated morbidity and soft tissue disruption. This surgical technique afforded a very satisfactory outcome for this patient and serves as a model for others when encountering a similar injury pattern in a trauma patient. It is a procedure that can be performed safely, quickly, and with minimal complications for surgeons with experience in arthroscopy of the hip joint. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (5) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
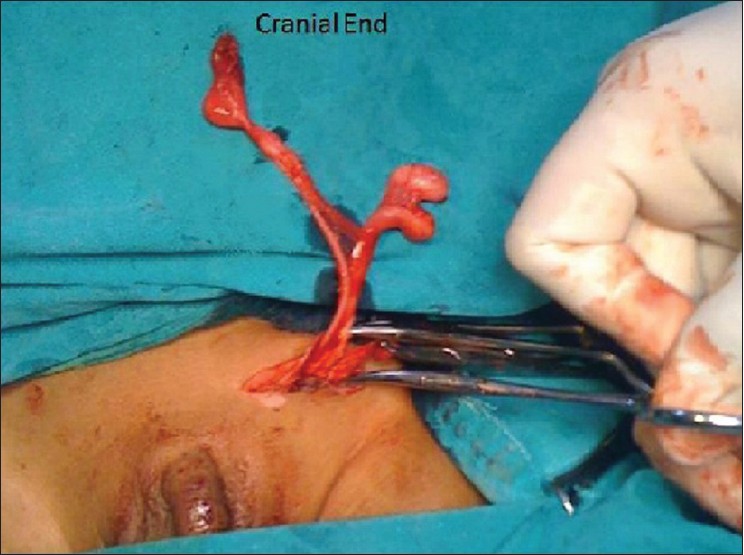  |
Triorchidism: A Rare Genitourinary Abnormality |
p. 126 |
Trupti Tonape, Gurjit Singh, P Koushik, Trinath Tumepalli
DOI:10.4103/2006-8808.110262 PMID:23741593Polyorchidism is an extremely rare congenital anomaly which refers to the presence of more than two testicles. There are very few reports of triorchidism in a 2 year old child. Polyorchidism is usually discovered incidentally. The most common anomalies associated with polyorchidism are inguinal hernia (30%), maldescended testis (15% to 30%), testicular torsion (13%) and hydrocele (9%). A 2-year-old child was brought with bilateral undescended testis with normal milestones. Ultrasonography of scrotum and abdomen showed both the testes to be in inguinal canal. Intra-operatively, on left side - there were two testes, which belonged to Leung III class and one testis on right side. Management of polyorchidism is still controversial. The management of polyorchidism will depend upon the location, size and anatomical organisation of the testicular drainage system and the age of the patient. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
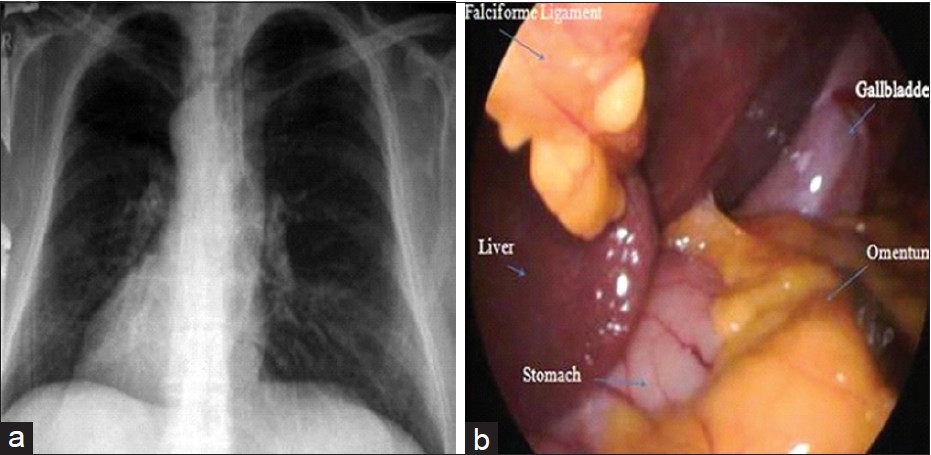  |
Single Incision Laparoscopic Cholecystectomy in situs Inversus Totalis |
p. 129 |
Suleyman Bozkurt, Halil Coskun, Tuba Atak, Huseyin Kadioglu
DOI:10.4103/2006-8808.110264 PMID:23741594Situs inversus totalis (SIT) is a rare genetic anomaly characterized by arrangement of the abdominal and thoracic organs in a perfect mirror image reversal of the normal positioning. Transposition of the organs causes difficulty in diagnosis and treatment of the diseases related to abdomen and thorax. Single incision laparoscopic surgery (SILS) is a new technique and it is increasingly used with better cosmetic results. In this paper, a single incision laparoscopic cholecystectomy (SILC) performed in a patient with SIT is presented. SILC can be performed safely in the patients with SIT with better cosmetic results. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (2) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
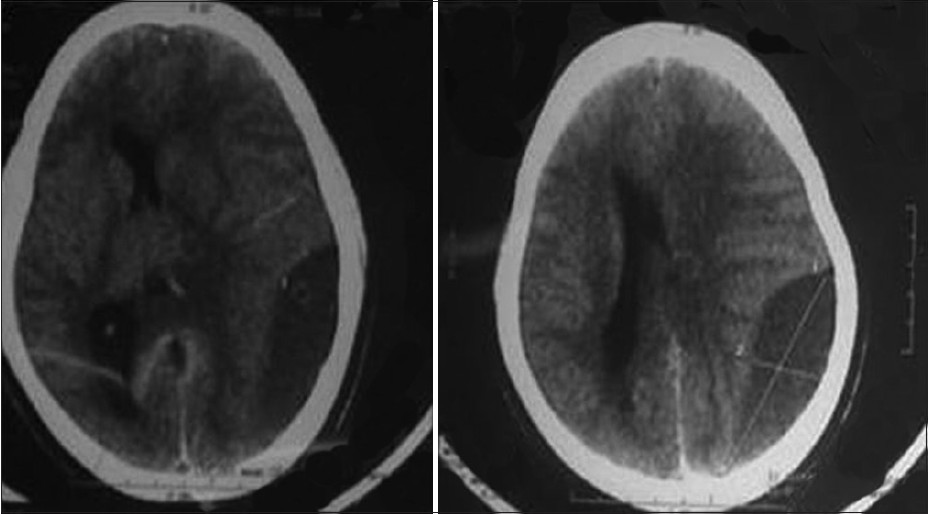  |
Management of Chronic Subdural Haematoma in a Case of Idiopathic Thrombocytopenic Purpura |
p. 132 |
Ashis Patnaik, Sudhansu S Mishra, Satya B Senapati, Acharya S Pattajoshi
DOI:10.4103/2006-8808.110265 PMID:23741595Intracranial hemorrhage is a rare devastating complication of idiopathic thrombocytopenic purpura (ITP), mostly presenting as intraparenchymal or subarachnoid haemorrhage. Isolated chronic subdural haematoma (SDH) is still very rare and the optimal management is unsettled. Spontaneous resolution of chronic SDH in patients with idiopathic thrombocytopenic purpura is possible. We report a case of spontaneous chronic SDH in a patient with ITP with hemiparesis where the haematoma significantly decreased in size with complete resolution of hemiparesis as a result of platelet transfusions and continuing therapy with steroids. Surgical treatment of subdural haematoma with consequent bleeding complications can be avoided in this scenario. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (2) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Spontaneous Epidural Haematoma in Sickle Cell Anaemia: Case Report and Literature Review |
p. 135 |
Bankole O Babatola, Yusuf A Salman, Asha M Abiola, Kanu O Okezie, Arigbabu S Oladele
DOI:10.4103/2006-8808.110271 PMID:23741596Non traumatic spontaneous epidural Haematoma is a rare and often unmentioned complication of sickle cell disease. It is often associated with skull bone infarction. We report an eighteen year old boy with sickle cell anaemia who developed persistence headache during a vaso-occlusive crisis. Brain computed tomography (CT) revealed a right frontal epidural Haematoma (EDH) compressing on the brain. No other etiologic factor was identified. A right frontal craniotomy and evacuation of the Haematoma was performed and he made good recovery. The possible pathogeneses of this rare condition are discussed. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| HOW I DO IT |
 |
|
|
  |
"Bilateral Double J Stent Removal: The way to do it!" |
p. 138 |
Rahul Yadav, Divakar Dalela, Neeraj K Goyal, Deepak Nagathan, Satya N Sankhwar
DOI:10.4103/2006-8808.110273 PMID:23741597There are many urological and non-urological indications which require bilateral double J stenting. We describe a point of technique for simultaneous removal of both the Double J stents. Both the stents are held by stent removing forceps at a point where they cross each other and then removed in one go with the help of cystoscope. Medline search did not reveal any techniques of removing two DJ stents in one go. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| LETTERS TO EDITOR |
 |
|
|
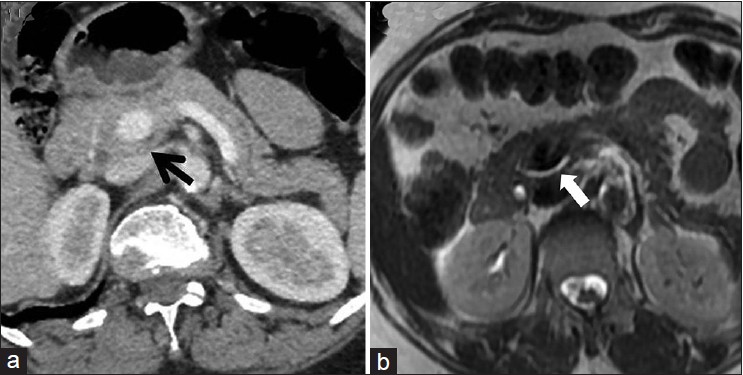  |
Portal Annular Pancreas: An Under-Reported Pancreatic Anomaly |
p. 140 |
Yashwant Patidar, Ankur Arora, Amar Mukund, Ankur Dev
DOI:10.4103/2006-8808.110272 PMID:23741598 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (3) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Management of Maternofetal Emergency in Shock with Fracture of Femur |
p. 141 |
Seema Rawat, Sanjay Meena
DOI:10.4103/2006-8808.110269 PMID:23741599 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|